Social Determinants of Mental Health
Mental health is significantly shaped by a complex interplay of social factors, extending beyond individual characteristics and genetics. Understanding these social determinants is crucial for developing effective preventative measures and reducing health disparities. This section explores key social factors influencing mental well-being, focusing on socioeconomic status, social support, and the impact of social inequality.
Socioeconomic Status and Mental Well-being
Socioeconomic status (SES), encompassing income, education, and occupation, profoundly impacts mental health outcomes. Individuals from lower SES backgrounds experience significantly higher rates of mental illness compared to their higher SES counterparts. This disparity is attributable to several factors. Financial strain associated with low income can lead to increased stress, reduced access to healthcare and mental health services, and poorer living conditions, all contributing to poorer mental health. Limited educational opportunities may restrict access to information about mental health and coping mechanisms, while precarious employment situations can generate chronic stress and job insecurity. Research consistently demonstrates a strong correlation between lower SES and increased prevalence of depression, anxiety, and substance abuse disorders. For example, studies have shown that individuals living in poverty are more likely to experience symptoms of PTSD following traumatic events due to a lack of resources to cope and recover.
The Role of Social Support Networks in Mental Health
Strong social support networks are a critical buffer against mental health challenges. These networks provide individuals with emotional, practical, and informational support, fostering a sense of belonging and reducing feelings of isolation and loneliness. Social connections offer opportunities for emotional regulation, stress management, and coping with adversity. Conversely, a lack of social support, characterized by social isolation or strained relationships, is a significant risk factor for mental health problems. Individuals lacking strong support systems are more vulnerable to the negative impacts of stress, life transitions, and traumatic events. For instance, elderly individuals living alone and lacking regular social interaction are at a higher risk for depression and cognitive decline. Conversely, participation in community groups, volunteering, and maintaining close relationships with family and friends has been shown to improve mental well-being across all age groups.
Social Inequality and Mental Health Disparities
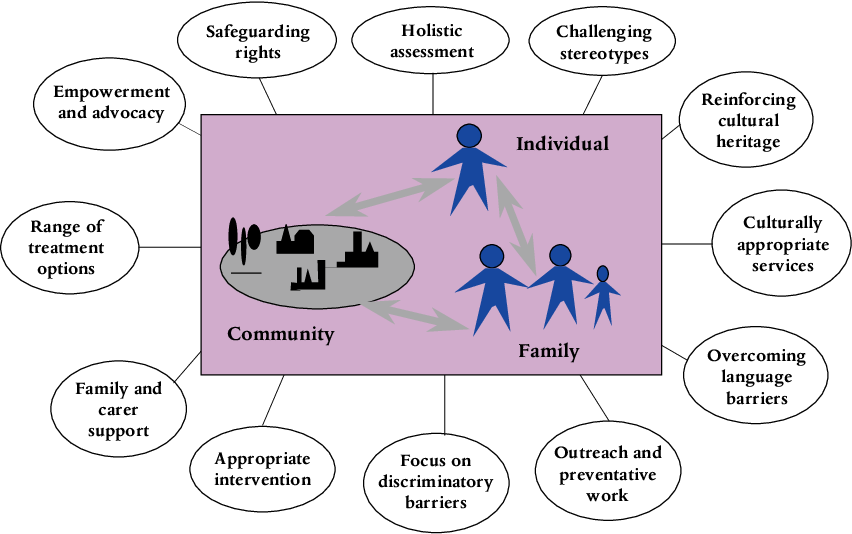
Social inequalities, such as discrimination based on race, ethnicity, gender, sexual orientation, and disability, significantly contribute to mental health disparities. Experiences of prejudice, stigma, and marginalization create chronic stress and undermine mental well-being. For example, racial minorities often face systemic discrimination in housing, employment, and healthcare, increasing their vulnerability to mental health problems. Similarly, LGBTQ+ individuals may experience higher rates of anxiety and depression due to societal stigma and discrimination. These disparities are not simply a matter of individual vulnerability but are rooted in broader societal structures and power imbalances. The cumulative effect of these social stressors can lead to significant mental health burdens within marginalized communities. The impact of these inequalities is often exacerbated by a lack of culturally competent mental health services that are accessible and responsive to the specific needs of diverse populations.
Preventative Measures Addressing Social Determinants
Addressing social determinants of mental health requires a multi-pronged approach targeting societal inequalities and promoting social well-being. Effective preventative measures include:
- Reducing socioeconomic inequalities through policies aimed at increasing income equality, affordable housing, and access to quality education and employment opportunities.
- Strengthening social support networks through community-based initiatives that foster social connection and reduce social isolation.
- Implementing anti-discrimination policies and promoting social inclusion to combat prejudice and stigma.
- Increasing access to affordable and culturally competent mental health services for all populations.
- Promoting mental health literacy through public education campaigns to reduce stigma and improve understanding of mental health conditions.
Research Methods in Mental Health Sociology: Is Mental Health Sociology

Mental health sociology employs a diverse range of research methods to understand the complex interplay between social factors and mental well-being. Researchers utilize both qualitative and quantitative approaches, often in mixed-methods designs, to gain a comprehensive understanding of this multifaceted area. Ethical considerations are paramount throughout the research process, guiding data collection, analysis, and dissemination.
Qualitative Research Methods in Mental Health Sociology
Qualitative methods prioritize in-depth understanding of experiences and perspectives. These methods are particularly valuable in exploring the lived realities of individuals with mental health conditions and the social contexts that shape their experiences. They offer rich, nuanced data that can illuminate the complexities often missed by quantitative approaches.
- In-depth Interviews: These allow researchers to explore individual experiences and perspectives in detail, uncovering the complexities of mental health within specific social contexts. For instance, a researcher might conduct in-depth interviews with individuals experiencing homelessness and mental illness to understand their unique challenges and coping mechanisms.
- Focus Groups: These group discussions provide insights into shared experiences and perspectives. Focus groups can be used to explore the stigma surrounding mental illness within specific communities or to understand the experiences of family members supporting loved ones with mental health conditions.
- Ethnographic Studies: These involve immersive, long-term observation of social groups, providing rich contextual data. An ethnographer might live within a community to understand how social structures and cultural norms impact mental health and help-seeking behaviors.
- Narrative Analysis: This method focuses on the stories individuals tell about their experiences, exploring how these narratives shape their understanding of their mental health and their place in the world. Researchers might analyze personal accounts of recovery to understand the role of social support in the process.
Quantitative Research Methods in Mental Health Sociology, Is mental health sociology
Quantitative methods emphasize numerical data and statistical analysis to identify patterns and relationships. These methods are useful for identifying prevalence rates, risk factors, and the effectiveness of interventions on a larger scale.
- Surveys: Large-scale surveys can be used to gather data on mental health prevalence, risk factors, and help-seeking behaviors across diverse populations. For example, a national survey could assess the prevalence of depression among different age groups and socioeconomic strata.
- Epidemiological Studies: These studies track the incidence and distribution of mental health conditions within populations, identifying patterns and potential risk factors. Researchers might conduct an epidemiological study to investigate the relationship between social inequality and the prevalence of anxiety disorders.
- Statistical Analysis of Existing Data: Researchers can analyze existing datasets, such as hospital records or census data, to identify correlations between social factors and mental health outcomes. For example, researchers could analyze census data to investigate the relationship between neighborhood poverty and rates of suicide.
Ethical Considerations in Mental Health Research
Ethical considerations are paramount in mental health research. Researchers must prioritize the well-being and autonomy of participants.
- Informed Consent: Participants must be fully informed about the study’s purpose, procedures, and potential risks and benefits before agreeing to participate. This is especially crucial when dealing with vulnerable populations.
- Confidentiality and Anonymity: Researchers must protect the privacy of participants by ensuring confidentiality and anonymity of their data. Data should be securely stored and analyzed in ways that protect participant identities.
- Minimizing Harm: Researchers must take steps to minimize any potential harm to participants, including emotional distress. This may involve providing access to support services or ensuring that the research process does not exacerbate existing mental health challenges.
- Beneficence and Non-Maleficence: Research should strive to benefit participants and avoid causing harm. This requires careful consideration of the potential impacts of the research on individuals and communities.
Effective Research Designs for Studying Mental Health in Social Contexts
Effective research designs often incorporate mixed methods, combining qualitative and quantitative approaches to provide a comprehensive understanding. Longitudinal studies, which track participants over time, can provide valuable insights into the dynamic interplay between social factors and mental health trajectories.
Hypothetical Research Project: The Impact of Social Isolation on Mental Well-being Among Older Adults
This project would investigate the relationship between social isolation and mental well-being among older adults living in a specific urban community. The study would employ a mixed-methods approach. Quantitative data would be collected through surveys measuring levels of social isolation and mental well-being (e.g., depression, anxiety). Qualitative data would be gathered through in-depth interviews with a subset of participants to explore their lived experiences of social isolation and its impact on their mental health. The data would then be analyzed to identify patterns and relationships, providing insights into the social determinants of mental health among older adults and informing the development of targeted interventions. Ethical considerations would be central throughout the research process, ensuring informed consent, confidentiality, and minimizing potential harm to participants.
Mental Health in Specific Social Contexts
Mental health disparities are significantly influenced by social context. Understanding the unique challenges faced by various populations is crucial for developing effective and equitable mental health interventions. This section will examine mental health issues within specific social groups, analyzing the contributing social factors and highlighting successful intervention strategies.
Mental Health Challenges Among Immigrants
Immigrants often face a complex interplay of stressors that negatively impact their mental well-being. These include the challenges of adapting to a new culture, language barriers, navigating a new healthcare system, and experiencing discrimination or xenophobia. Furthermore, separation from family and social support networks, financial instability, and the trauma of migration itself can contribute to higher rates of anxiety, depression, and post-traumatic stress disorder (PTSD). Successful interventions often involve culturally sensitive care, bilingual services, and community-based support programs that address the specific needs of immigrant populations. For example, peer support groups led by individuals with shared immigration experiences can provide valuable emotional support and practical advice.
Mental Health and the LGBTQ+ Community
Members of the LGBTQ+ community experience significantly higher rates of mental health disorders compared to the general population. This disparity is linked to various factors, including discrimination, stigma, and societal prejudice. Minority stress, a concept describing the chronic stress associated with being a member of a marginalized group, plays a significant role. This stress can stem from experiences such as harassment, bullying, violence, and lack of legal protections. Furthermore, difficulties in accessing affirming healthcare providers and a lack of inclusive mental health services contribute to the problem. Effective interventions focus on creating safe and inclusive spaces, providing culturally competent care, and addressing the specific needs and concerns of LGBTQ+ individuals. Examples include specialized LGBTQ+-affirming therapy and community-based organizations offering support and resources.
Mental Health in Incarcerated Populations
Incarcerated individuals face exceptionally high rates of mental illness, often exacerbated by the conditions of confinement and the trauma associated with the criminal justice system. Factors contributing to poor mental health include exposure to violence, substance abuse, lack of access to adequate healthcare, and social isolation. The stigma associated with mental illness within the prison system can also hinder individuals from seeking help. Effective interventions require a multifaceted approach, including improved access to mental healthcare within correctional facilities, trauma-informed care, and programs focused on relapse prevention and reintegration into the community upon release. Examples include providing medication management, individual and group therapy, and vocational training to support successful reentry.
Comparative Analysis of Mental Health Outcomes
| Social Group | Common Mental Health Challenges | Contributing Social Factors | Examples of Successful Interventions |
|---|---|---|---|
| Immigrants | Anxiety, Depression, PTSD | Cultural adjustment, language barriers, discrimination | Culturally sensitive therapy, bilingual services, peer support groups |
| LGBTQ+ Individuals | Anxiety, Depression, PTSD, Substance Abuse | Discrimination, stigma, minority stress | LGBTQ+-affirming therapy, inclusive community centers, safe spaces |
| Incarcerated Individuals | Depression, Anxiety, PTSD, Substance Abuse | Violence exposure, lack of healthcare access, social isolation | Improved access to healthcare, trauma-informed care, reintegration programs |

Tim Redaksi