Defining CSPS Mental Health
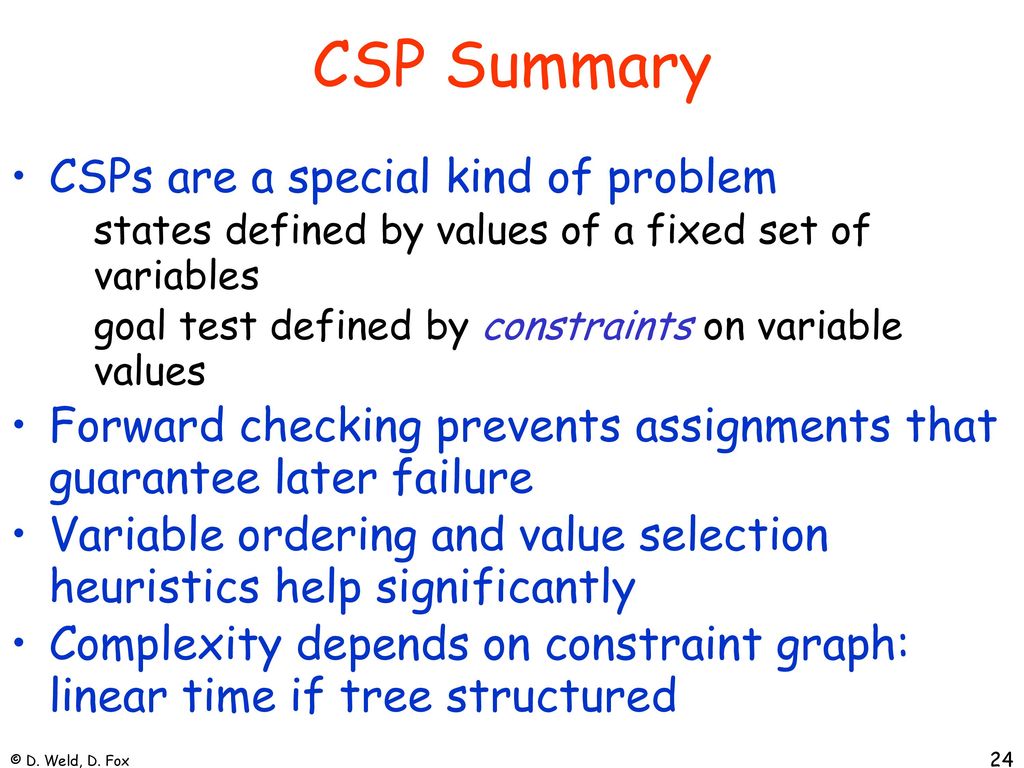
Community Support Programs and Services (CSPS) mental health focuses on providing integrated, person-centered care within the individual’s natural environment, aiming for recovery and improved quality of life. It differs significantly from traditional, more institutionalized models of mental healthcare.
Core Components of CSPS Mental Health
CSPS mental health incorporates several key components. These include individualized support planning, emphasizing the person’s strengths and goals; collaborative care involving various professionals and the individual; community-based services, minimizing institutionalization; and a focus on skills development and empowerment, promoting self-management and independence. A strong emphasis is placed on social inclusion and reducing stigma associated with mental illness. The overall aim is to support individuals in living fulfilling lives within their communities.
Challenges Faced by Individuals Receiving CSPS Mental Health Support
Individuals accessing CSPS mental health services often face unique challenges. These can include navigating a complex system of services, securing adequate funding for support, experiencing stigma and discrimination within their communities, managing co-occurring disorders (substance abuse, physical health problems), and maintaining consistent engagement with services due to logistical barriers or personal circumstances. Furthermore, access to specialized care may be limited depending on geographical location and the availability of resources within the community.
Comparison of CSPS Mental Health Services with Other Models
CSPS mental health contrasts with traditional hospital-based inpatient care, which is often more intensive and restrictive. It also differs from purely medication-focused outpatient care, which may lack the holistic and integrated approach of CSPS. Compared to case management alone, CSPS provides a broader range of services and a more comprehensive support system. The key differentiator is the emphasis on community integration, person-centered planning, and collaborative care. While traditional models may focus primarily on symptom reduction, CSPS prioritizes recovery, social inclusion, and improved overall well-being.
Common Mental Health Conditions Addressed by CSPS
CSPS programs address a wide range of mental health conditions. Common examples include depression, anxiety disorders (generalized anxiety disorder, panic disorder, social anxiety disorder), bipolar disorder, schizophrenia, post-traumatic stress disorder (PTSD), and substance use disorders. The specific services provided are tailored to the individual’s needs and diagnosis.
Types of CSPS Mental Health Interventions
The following table illustrates different types of CSPS mental health interventions, their target populations, key features, and limitations:
| Intervention Type | Target Population | Key Features | Limitations |
|---|---|---|---|
| Individual Therapy | Individuals with various mental health conditions | Personalized support, tailored interventions, focus on coping skills | Can be expensive, requires commitment from the individual |
| Group Therapy | Individuals with similar mental health conditions | Peer support, shared experiences, cost-effective | May not be suitable for all individuals, group dynamics can be challenging |
| Case Management | Individuals needing assistance navigating the mental health system | Coordination of services, advocacy, resource linkage | Workload can be heavy, caseloads may be large |
| Supported Employment | Individuals with mental illness seeking employment | Job coaching, workplace support, skill development | Job availability, competition for positions |
Types of CSPS Mental Health Interventions
CSPS (Child and Adolescent Services Psychiatry) mental health interventions are multifaceted, drawing upon various therapeutic approaches tailored to the unique needs of young people. Effective treatment requires a comprehensive understanding of the individual’s developmental stage, presenting concerns, and overall context. The interventions described below highlight the diverse strategies employed to promote mental well-being in this population.
Therapeutic Approaches in CSPS Settings
A range of therapeutic approaches are utilized within CSPS settings, each offering distinct advantages depending on the specific mental health condition and individual needs. Cognitive Behavioral Therapy (CBT) focuses on identifying and modifying maladaptive thoughts and behaviors. Dialectical Behavior Therapy (DBT), often used for individuals with borderline personality disorder or self-harming behaviors, emphasizes emotional regulation and distress tolerance skills. Psychodynamic therapy explores unconscious patterns and past experiences to understand current difficulties. Other approaches, such as family therapy and play therapy (for younger children), are also frequently incorporated to address the broader systemic factors influencing a young person’s mental health.
Effectiveness of Interventions for Specific Conditions, What is a csps mental health
The effectiveness of different interventions varies depending on the specific mental health condition. For example, CBT has demonstrated strong evidence-based support for treating anxiety disorders and depression in adolescents. DBT has proven particularly effective in reducing suicidal ideation and self-harm in individuals with borderline personality disorder. Psychodynamic therapy can be helpful in addressing long-standing emotional issues and relationship patterns, although its effectiveness may be more challenging to quantify compared to empirically supported therapies like CBT. The choice of intervention is often guided by clinical assessment, considering the individual’s diagnosis, symptoms, strengths, and preferences.
The Role of Medication Management in CSPS Mental Health Care
Medication management plays a significant role in CSPS mental health care, often used in conjunction with psychotherapy. Psychotropic medications can help manage symptoms of various mental health conditions, such as depression, anxiety, psychosis, and attention-deficit/hyperactivity disorder (ADHD). A psychiatrist or other qualified medical professional prescribes and monitors medication, carefully considering potential side effects and interactions. Regular monitoring of medication effectiveness and side effects is crucial to ensure optimal treatment outcomes and patient safety. Medication is rarely a standalone treatment; it’s typically part of a broader treatment plan that includes psychotherapy and other supportive services.
Hypothetical CSPS Program for Anxiety Disorders
A hypothetical CSPS program focusing on anxiety disorders in adolescents (ages 13-18) might incorporate several key components. The program would begin with a comprehensive assessment to determine the type and severity of anxiety, along with any co-occurring conditions. CBT would be the primary therapeutic intervention, with sessions focusing on cognitive restructuring, exposure therapy, and relaxation techniques. Group therapy would provide a supportive environment for sharing experiences and learning coping skills. Parents or guardians would be involved in family sessions to understand the adolescent’s experience and learn how to support them effectively. The program would also incorporate educational components about anxiety and stress management, as well as relapse prevention strategies.
Supportive Services in CSPS
Therapeutic interventions are often complemented by supportive services designed to address the broader context of a young person’s life. These services might include housing assistance for those experiencing homelessness or instability, employment support to help adolescents gain vocational skills and find employment, and substance abuse treatment for those struggling with substance use disorders. School liaison services can facilitate communication between the CSPS team and the school, ensuring a consistent and supportive environment for the adolescent. Access to nutritional counseling and physical activity programs can also be beneficial, promoting overall physical and mental well-being. The integration of these supportive services enhances the effectiveness of therapeutic interventions by addressing the multiple factors influencing a young person’s mental health.
Outcomes and Evaluation of CSPS Mental Health Services
Effective evaluation is crucial for ensuring CSPS mental health programs achieve their intended goals and improve the well-being of clients. A robust evaluation framework allows for the identification of successful strategies, areas needing improvement, and the overall impact of interventions. This section details methods for evaluating the effectiveness of CSPS mental health services, focusing on data collection, key indicators, and the importance of ongoing program adaptation.
Methods for Evaluating CSPS Mental Health Program Effectiveness
Evaluating the effectiveness of CSPS mental health programs requires a multifaceted approach employing various metrics. Quantitative data, such as symptom reduction scores and service utilization rates, provide objective measures of program impact. Qualitative data, gathered through client feedback and staff observations, offer valuable insights into the client experience and the program’s strengths and weaknesses. A combined approach allows for a comprehensive understanding of program effectiveness. For instance, measuring changes in standardized depression scales (e.g., PHQ-9) alongside qualitative feedback on program satisfaction can provide a more complete picture of outcomes.
Data Collection Methods for Assessing Client Outcomes
Several data collection methods are used to assess client outcomes in CSPS mental health settings. These include: self-report questionnaires (measuring symptoms, functioning, and satisfaction); clinician-administered assessments (providing objective measures of mental health status); progress notes documenting clinical observations and treatment progress; and administrative data (tracking service utilization, length of treatment, and client demographics). Combining these methods offers a rich dataset for comprehensive analysis. For example, tracking attendance rates alongside self-reported symptom severity can indicate engagement and treatment response.
Key Indicators of Success in CSPS Mental Health Interventions
Key indicators of success in CSPS mental health interventions vary depending on the specific program goals. However, some common indicators include: statistically significant reductions in symptom severity (as measured by standardized scales); improvements in functional capacity (e.g., work, social, and daily living skills); increased client satisfaction with services; reduced hospitalizations or emergency room visits; and improved quality of life as reported by clients. The successful implementation of a program that results in a significant reduction in reported suicidal ideation would be a notable indicator of success.
Importance of Ongoing Evaluation and Program Adaptation
Ongoing evaluation is essential for continuous quality improvement in CSPS mental health services. Regular monitoring of key indicators allows for timely identification of areas needing improvement. This ongoing data analysis informs program adaptations, ensuring services remain relevant, effective, and responsive to client needs. For instance, if client feedback consistently highlights a need for more flexible scheduling, program modifications can be implemented to address this need.
Potential Outcome Measures for CSPS Mental Health Programs
| Outcome Measure | Data Source | Method of Measurement | Interpretation |
|---|---|---|---|
| Symptom Severity (e.g., Depression, Anxiety) | Self-report questionnaires, clinician assessments | Standardized scales (PHQ-9, GAD-7) | Changes in scores over time indicate improvement or deterioration. |
| Functional Capacity | Self-report questionnaires, clinician observations, functional assessments | Scales measuring daily living skills, work productivity, social functioning | Improvements reflect increased ability to perform daily tasks and engage in social activities. |
| Client Satisfaction | Client surveys, feedback sessions | Rating scales, open-ended questions | High satisfaction scores indicate positive client experiences. |
| Service Utilization | Administrative data | Number of sessions attended, length of treatment | High utilization suggests engagement with services; low utilization may indicate barriers to access. |
Ethical Considerations in CSPS Mental Health: What Is A Csps Mental Health
Providing mental health services within the correctional system (CSPS) presents a unique set of ethical challenges, demanding careful consideration and proactive strategies to ensure the well-being and rights of incarcerated individuals. These challenges stem from the inherent power imbalance between staff and inmates, the restrictive environment, and the complex interplay of legal and ethical obligations. Effective ethical practice requires a commitment to upholding professional standards while navigating the realities of the correctional setting.
Informed Consent and Client Autonomy in CSPS Mental Health Settings
Informed consent, a cornerstone of ethical practice, requires that individuals understand the nature of the treatment, its potential benefits and risks, and their right to refuse or withdraw from services at any time. In CSPS, obtaining truly informed consent can be complicated. Individuals may feel coerced into treatment due to their incarceration, or their cognitive abilities may be impaired by mental illness or substance abuse. Clinicians must therefore take extra care to ensure that consent is voluntary, informed, and ongoing, actively addressing any potential power imbalances and ensuring clients understand their rights and options. This might involve using simplified language, providing multiple opportunities for questions and clarification, and involving family or legal representatives where appropriate. Furthermore, documenting the informed consent process meticulously is crucial for accountability and legal protection.
Confidentiality and Privacy Protection in CSPS Mental Health Care
Maintaining confidentiality is paramount in any therapeutic relationship. However, the CSPS context presents unique challenges. Legal mandates often require disclosure of information to correctional staff for security reasons or to prevent harm. Balancing the need for confidentiality with the requirements of the correctional setting requires careful navigation of legal and ethical boundaries. Clinicians must be knowledgeable about relevant laws and policies, and they must establish clear protocols for information sharing, ensuring that only necessary information is disclosed and only to authorized personnel. The use of secure electronic health records and appropriate safeguards for physical files are also essential to protect client privacy. Open communication with clients about the limits of confidentiality is crucial, fostering trust and transparency.
Ethical Decision-Making Models in CSPS Mental Health Practice
Various ethical decision-making models can guide professionals in navigating complex situations within CSPS mental health. The principle-based approach, focusing on autonomy, beneficence, non-maleficence, and justice, provides a framework for evaluating potential courses of action. The utilitarian approach, which emphasizes maximizing overall good, can also be relevant, particularly when considering resource allocation or public safety. However, a purely utilitarian approach must be balanced with individual rights. A virtue ethics approach, emphasizing the character and moral integrity of the clinician, is also important. In practice, a combination of these models often proves most effective, allowing clinicians to consider multiple perspectives and arrive at ethically sound decisions.
Examples of Ethical Dilemmas and Potential Resolutions in CSPS Mental Health
A common ethical dilemma arises when a client discloses information about a planned escape or potential harm to others. The clinician must balance the duty to maintain confidentiality with the legal and ethical obligation to protect the safety of others. This requires careful consideration of the severity of the threat, the likelihood of harm, and the availability of alternative strategies. Reporting to correctional authorities may be necessary, but it should be done in a manner that minimizes further harm to the client’s therapeutic relationship and respects their dignity as much as possible. Another example involves managing medication compliance. While medication can be crucial for managing mental illness, involuntary medication raises significant ethical concerns regarding autonomy. Clinicians must carefully weigh the benefits of medication against the potential infringement on individual rights, considering alternatives and engaging in collaborative decision-making wherever possible. Thorough documentation of the decision-making process is vital in both scenarios.

Tim Redaksi