Lessons Learned and Prevention Strategies: How Did Heritage Valley Health System Get Hacked

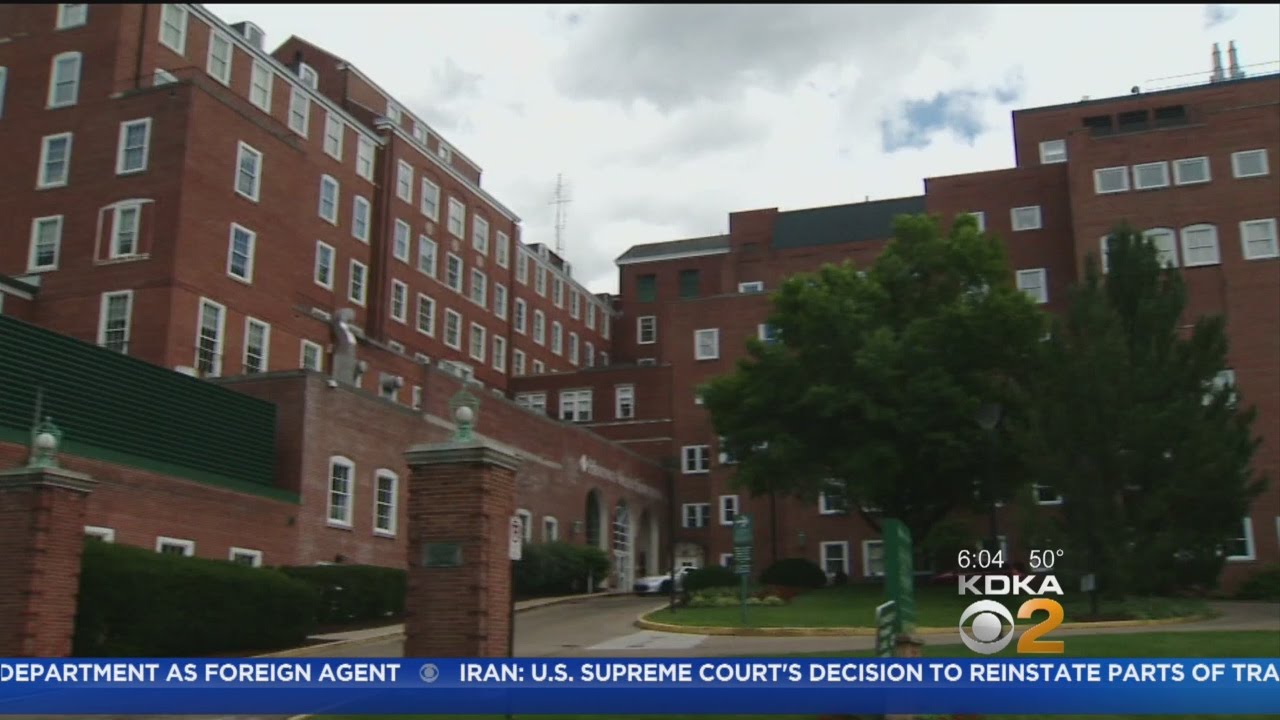
The Heritage Valley Health System data breach highlighted critical vulnerabilities in healthcare cybersecurity. Analyzing this incident reveals valuable insights for improving security protocols and preventing future attacks. Understanding the weaknesses exploited and implementing robust preventative measures are paramount to safeguarding patient data and maintaining public trust.
The incident underscores the need for a multi-faceted approach to cybersecurity, encompassing technological safeguards, rigorous employee training, and proactive risk management. A comprehensive strategy must be adaptable and continuously updated to address the evolving threat landscape.
Key Lessons Learned from the Heritage Valley Breach
The Heritage Valley breach, while specific in its details, offers several universal lessons applicable across healthcare organizations. These lessons emphasize the interconnectedness of various security components and the importance of holistic risk management. Failure in one area can compromise the entire system. For example, insufficient employee training on phishing techniques directly contributed to the initial access point for the attackers. Furthermore, inadequate network segmentation allowed the attackers to move laterally within the system, accessing more sensitive data than initially anticipated. Finally, a lack of robust monitoring and detection systems delayed the identification of the breach, extending the window of vulnerability.
Best Practices for Healthcare Cybersecurity, How did heritage valley health system get hacked
Effective cybersecurity in healthcare requires a layered approach combining technological solutions, robust policies, and comprehensive employee training. This approach aims to minimize the risk of data breaches and ensure the confidentiality, integrity, and availability of sensitive patient information. Healthcare organizations should prioritize regular security assessments, penetration testing, and vulnerability scanning to identify and mitigate potential threats proactively. Furthermore, implementing strong access controls, including multi-factor authentication, and regularly updating software and systems are crucial steps. A comprehensive incident response plan, regularly tested and updated, is essential to minimize the impact of a successful attack.
Preventative Measures for Healthcare Organizations
A proactive approach to cybersecurity requires a combination of strategies focused on people, processes, and technology.
- Employee Training: Regular and comprehensive security awareness training for all employees is critical. This should include phishing simulations, safe password practices, and data handling procedures. Training should be tailored to different roles and responsibilities within the organization, focusing on the specific threats relevant to each position.
- System Updates and Patching: Promptly applying software updates and security patches is essential to address known vulnerabilities. Organizations should establish a robust patch management system to ensure timely updates across all systems and devices.
- Security Audits and Assessments: Regular security audits and vulnerability assessments are crucial for identifying weaknesses in the organization’s security posture. These assessments should be conducted by qualified professionals and should cover all aspects of the IT infrastructure, including network security, application security, and data security.
- Data Loss Prevention (DLP) Measures: Implementing DLP tools can help prevent sensitive data from leaving the organization’s control. These tools can monitor data movement and prevent unauthorized access or transfer of protected health information (PHI).
- Network Segmentation: Dividing the network into smaller, isolated segments can limit the impact of a breach. If one segment is compromised, the attackers will have limited access to other parts of the network.
- Multi-Factor Authentication (MFA): Requiring MFA for all users, especially those with access to sensitive data, significantly strengthens account security and makes it more difficult for attackers to gain unauthorized access.
- Incident Response Plan: A well-defined and regularly tested incident response plan is crucial for handling security incidents effectively. This plan should Artikel procedures for identifying, containing, and remediating security breaches.
Legal and Regulatory Implications

The Heritage Valley Health System data breach carried significant legal and regulatory ramifications, primarily stemming from violations of the Health Insurance Portability and Accountability Act (HIPAA). Failure to adequately safeguard Protected Health Information (PHI) resulted in potential legal liabilities and substantial financial penalties. The breach also triggered reputational damage, impacting patient trust and the overall stability of the healthcare system.
HIPAA Violations and Potential Lawsuits
The breach likely resulted in several HIPAA violations, specifically those related to the security and privacy rules. These rules mandate the implementation of reasonable and appropriate safeguards to protect PHI from unauthorized access, use, or disclosure. Failure to meet these standards could lead to significant fines from the Office for Civil Rights (OCR), which enforces HIPAA compliance. Furthermore, affected patients could pursue legal action against Heritage Valley, claiming damages for identity theft, emotional distress, or other harms resulting from the exposure of their PHI. Class-action lawsuits are a common outcome in such situations, potentially resulting in substantial financial settlements or judgments. The legal costs associated with defending against these lawsuits would further burden the healthcare system.
Financial and Reputational Consequences
The financial repercussions of the breach extend beyond potential fines and legal settlements. Heritage Valley likely faced increased cybersecurity insurance premiums and the cost of implementing improved security measures to prevent future breaches. These costs can be substantial, especially for a large healthcare system. Beyond the direct financial losses, the reputational damage caused by the breach can be equally devastating. Loss of patient trust can lead to a decline in patient volume, impacting revenue and the long-term viability of the system. Negative media coverage and public perception can also damage the organization’s reputation within the broader healthcare community, making it harder to attract and retain skilled professionals.
Impact on Patient Trust and Confidence
A data breach severely erodes patient trust and confidence in a healthcare provider. Patients entrust their sensitive health information to healthcare organizations, expecting it to be protected. When a breach occurs, this trust is broken, leading to anxiety and uncertainty. Patients may become hesitant to seek care from the compromised organization, fearing further breaches or misuse of their information. Rebuilding this trust requires a transparent and proactive approach from Heritage Valley, including open communication with affected patients, detailed explanations of the breach and the steps taken to address it, and demonstrable improvements in data security practices. The long-term impact on patient relationships and the organization’s reputation is difficult to quantify but could be significant.
Impact on Patients and Employees
A data breach at a healthcare system like Heritage Valley Health System can have devastating consequences for both patients and employees, extending far beyond the immediate disruption of services. The potential for identity theft, financial losses, and reputational damage is significant and long-lasting. Understanding these potential impacts is crucial for assessing the overall severity of such an event and implementing effective preventative measures.
The potential ramifications for patients are particularly concerning given the sensitive nature of their protected health information (PHI). This information, often including medical history, insurance details, and financial data, is highly valuable to identity thieves and can be used for a range of malicious activities.
Patient Impacts
A data breach could lead to several serious consequences for patients. Identity theft, including medical identity theft, is a major concern. Medical identity theft can result in the patient being denied treatment or incurring significant debt due to fraudulent claims filed in their name. Financial loss can also occur through unauthorized access to banking details or insurance information. Furthermore, the emotional distress and time investment required to rectify the situation after a breach can be substantial. For example, the 2015 Anthem breach, affecting nearly 80 million individuals, resulted in numerous cases of identity theft and significant financial losses for affected patients, requiring extensive monitoring and credit repair services.
Employee Impacts
The impact on employees is equally significant, extending beyond potential financial losses. A data breach can lead to loss of employment, particularly if the breach is attributed to negligence on the part of an employee. Even without job loss, reputational damage can be considerable, potentially affecting future employment prospects. Employees may also face financial losses due to identity theft or the need to take time off work to address the aftermath of the breach. Furthermore, the stress and anxiety associated with a data breach can have a profound impact on employee well-being. Similar breaches at other healthcare organizations have shown that employees can experience significant emotional distress, leading to decreased productivity and increased healthcare costs for the organization. The Premera Blue Cross breach in 2015, for instance, not only impacted millions of customers but also resulted in significant stress and anxiety among employees involved in the aftermath of the incident.

Tim Redaksi