Oral Health and Cardiovascular Disease
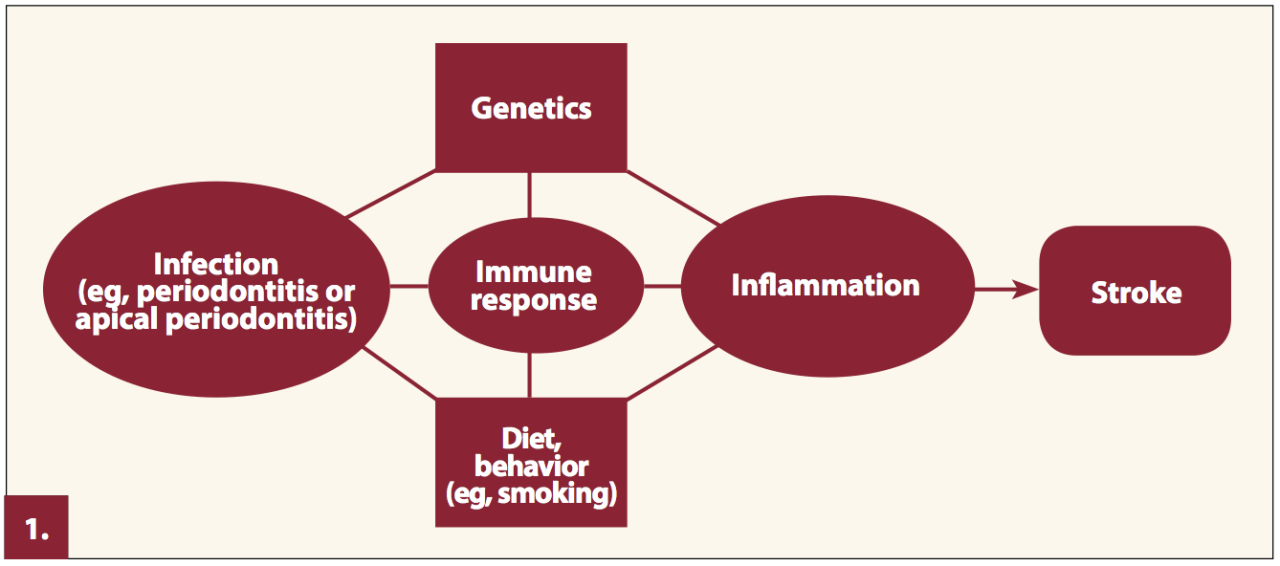
The connection between oral health and cardiovascular disease (CVD), including stroke, is increasingly recognized by the medical community. While not a direct cause-and-effect relationship in all cases, accumulating evidence strongly suggests that poor oral hygiene and specific oral diseases significantly elevate the risk of developing CVD. This relationship is complex and multifaceted, involving several interconnected pathways.
Poor oral health can contribute to systemic inflammation throughout the body. This chronic inflammation is a key factor in the development and progression of atherosclerosis, the underlying cause of many cardiovascular events, including stroke. The mechanisms linking oral health to stroke are not fully elucidated, but several pathways are implicated.
Mechanisms Linking Poor Oral Health to Stroke Risk
Bacteria and their byproducts from periodontal disease can enter the bloodstream, triggering inflammatory responses that damage blood vessels. This process can lead to the formation of blood clots, a major contributor to stroke. Furthermore, chronic inflammation associated with gum disease can increase the stickiness of platelets, making them more likely to form clots. The resulting plaque buildup in arteries can restrict blood flow to the brain, leading to ischemic stroke. Conversely, inflammation can also contribute to hemorrhagic stroke by weakening blood vessel walls, making them more prone to rupture.
Oral Health Conditions Increasing Stroke Risk
Periodontal disease, characterized by inflammation and infection of the gums and supporting tissues of the teeth, is the most significant oral health condition linked to increased stroke risk. Untreated gingivitis (gum inflammation) can progress to periodontitis, a more severe form of gum disease, leading to tooth loss and bone damage. The chronic inflammation associated with these conditions contributes to systemic inflammation, increasing the risk of stroke. Other oral conditions, such as oral infections and poor oral hygiene, can also contribute to elevated stroke risk by similar mechanisms.
Risk Factors for Oral Disease and Stroke: A Comparison
| Risk Factor | Oral Disease | Stroke | Shared Mechanisms |
|---|---|---|---|
| Age | Increased risk with age due to weakened immune system and reduced saliva production. | Increased risk with age due to vascular aging and other comorbidities. | Age-related physiological changes contribute to both conditions. |
| Smoking | Reduces blood supply to gums, increasing susceptibility to infection. | Damages blood vessels, increases blood pressure, and promotes blood clot formation. | Direct vascular damage and inflammation. |
| Diabetes | Impairs immune function, making individuals more vulnerable to gum disease. | Damages blood vessels, increases risk of blood clots, and contributes to atherosclerosis. | Impaired immune function and vascular damage. |
| High Blood Pressure | Less directly linked but can contribute to overall inflammation. | Major risk factor; increases stress on blood vessels and risk of rupture or blockage. | Contribution to systemic inflammation and vascular damage. |
Role of Oral Health Personnel in Screening and Early Detection
Oral health professionals, particularly dental hygienists, are uniquely positioned to play a significant role in the early detection of individuals at high risk for stroke. Their regular contact with patients, coupled with the close relationship between oral and systemic health, provides an ideal opportunity for incorporating stroke risk assessment into routine dental care. This proactive approach can contribute significantly to early intervention and improved patient outcomes.
Dental hygienists, through their comprehensive oral examinations, can identify several indicators that may suggest an increased risk of stroke. This early identification allows for timely referrals to primary care physicians, facilitating appropriate management and preventative strategies. By integrating stroke risk assessment into their practice, dental hygienists can become vital partners in stroke prevention efforts.
Identifying High-Risk Individuals, A role for oral health personnel in stroke prevention.
Dental hygienists can identify individuals at high risk for stroke by observing specific oral manifestations and gathering relevant patient history. This includes assessing factors such as periodontal disease severity, presence of oral bleeding, and the patient’s self-reported medical history, including hypertension, diabetes, and smoking status. Furthermore, careful observation of the oral mucosa for signs of inflammation or unusual lesions can provide valuable clues. A thorough understanding of cardiovascular risk factors is crucial for effective screening.
Incorporating Stroke Risk Assessment into Routine Examinations
Best practices for incorporating stroke risk assessment into routine dental examinations involve a multi-faceted approach. First, a brief, targeted questionnaire should be administered to gather essential information regarding cardiovascular risk factors. Second, a visual inspection of the oral cavity should be conducted, looking for potential indicators of systemic disease. Third, a discussion of the patient’s overall health and lifestyle should be initiated, encouraging open communication about potential risk factors. Finally, appropriate referrals to primary care physicians should be made for patients identified as being at high risk. This integrated approach maximizes the effectiveness of stroke risk screening within the dental setting.
Simple Stroke Risk Screening Questionnaire
The following questionnaire can be easily incorporated into routine dental examinations:
| Question | Yes/No/Unsure |
|---|---|
| Do you have high blood pressure (hypertension)? | |
| Do you have diabetes? | |
| Do you smoke or use tobacco products? | |
| Do you have a family history of stroke? | |
| Do you have high cholesterol? | |
| Do you have a history of heart disease? | |
| Do you experience frequent headaches or dizziness? |
This questionnaire provides a quick assessment of key risk factors. A “yes” answer to several questions may warrant a referral to a primary care physician for further evaluation.
Visible Oral Manifestations Indicating Cardiovascular Issues
Several visible oral manifestations can indicate underlying cardiovascular issues. These include:
- Severe periodontal disease: Extensive gum inflammation and bone loss are associated with increased risk of cardiovascular events.
- Oral bleeding: Excessive bleeding during dental procedures or spontaneous bleeding may indicate clotting disorders.
- Oral manifestations of atherosclerosis: Lesions or discolorations of the oral mucosa can sometimes be indicative of atherosclerosis.
- Presence of oral infections: Untreated oral infections can contribute to systemic inflammation, increasing cardiovascular risk.
It is important to remember that the presence of these oral manifestations does not definitively diagnose cardiovascular disease but rather warrants further investigation and potential referral to a physician.
Oral Health Interventions and Stroke Prevention: A Role For Oral Health Personnel In Stroke Prevention.

Improved oral hygiene and periodontal treatment offer significant potential for reducing stroke risk. The connection between oral and systemic health is increasingly recognized, highlighting the crucial role oral health professionals play in broader preventative healthcare strategies. This section explores specific interventions and educational resources to integrate into stroke prevention programs.
A role for oral health personnel in stroke prevention. – Maintaining good oral hygiene significantly reduces the risk of periodontal disease, a chronic inflammatory condition affecting the gums and supporting structures of the teeth. Research suggests a strong link between periodontal disease and increased risk of cardiovascular events, including stroke. This is likely due to the systemic inflammatory response triggered by periodontal pathogens, which can contribute to atherosclerosis (hardening of the arteries) and the formation of blood clots – key factors in stroke development. Improved oral hygiene practices, such as regular brushing and flossing, can help control inflammation and reduce the bacterial load in the mouth, potentially mitigating this risk.
Impact of Periodontal Treatment on Cardiovascular Health
Periodontal treatment, including scaling and root planing (professional cleaning to remove plaque and tartar below the gum line), can effectively manage periodontal disease and its associated inflammation. Studies have demonstrated that successful periodontal treatment can lead to improvements in cardiovascular health markers, such as reduced C-reactive protein (CRP), a marker of inflammation. This reduction in systemic inflammation can, in turn, contribute to a lower risk of cardiovascular events, including stroke. For instance, a study published in the Journal of Clinical Periodontology showed a statistically significant reduction in cardiovascular events among patients who received periodontal treatment compared to those who did not. The improved cardiovascular health outcomes observed following periodontal treatment underscore the importance of integrating periodontal care into broader stroke prevention strategies.
Specific Oral Health Interventions for Stroke Prevention
Integrating oral health interventions into existing stroke prevention programs requires a multi-faceted approach. This includes promoting regular dental check-ups and professional cleanings, emphasizing the importance of good oral hygiene practices at home, and providing targeted interventions for individuals at high risk of both periodontal disease and stroke.
Specific interventions could include:
- Early detection and management of periodontal disease: Regular screenings for periodontal disease during routine dental check-ups are crucial. Early intervention can prevent the progression of the disease and reduce its impact on systemic health.
- Patient education on oral hygiene: Providing clear and concise instructions on proper brushing and flossing techniques, as well as emphasizing the importance of regular dental visits, is vital. This can be tailored to individual patient needs and risk factors.
- Referral to specialists: Oral health professionals should be equipped to identify patients who require referral to periodontists or other specialists for more advanced periodontal treatment.
- Collaboration with other healthcare providers: Close collaboration with physicians, cardiologists, and other healthcare professionals involved in stroke prevention is essential to ensure a coordinated and holistic approach to patient care.
Examples of Educational Materials for Stroke Prevention
Effective educational materials are crucial for promoting oral health and stroke prevention. These materials should be accessible, easy to understand, and tailored to different populations.
Examples of such materials include:
- Informative brochures and pamphlets: These can provide concise information about the link between oral health and stroke, emphasizing the importance of good oral hygiene and regular dental visits. Visual aids, such as diagrams and illustrations of proper brushing techniques, can enhance understanding.
- Educational videos: Short, engaging videos can demonstrate proper brushing and flossing techniques and explain the connection between oral health and stroke risk in a visually appealing manner. These can be easily shared online or shown in waiting rooms.
- Interactive online resources: Websites and apps can provide personalized information and tools to help individuals track their oral hygiene habits and access educational resources. These can include interactive quizzes and personalized recommendations.
- Community outreach programs: Collaborating with community organizations to offer oral health screenings and educational workshops can increase awareness and access to preventative care, particularly in underserved populations.
Collaboration and Interprofessional Care
Effective stroke prevention requires a collaborative approach, integrating the expertise of various healthcare professionals. Oral health professionals possess unique insights into a patient’s overall health, contributing significantly to early detection and prevention strategies. Their collaboration with physicians and other healthcare providers is crucial for optimizing patient outcomes.
Oral health professionals and other healthcare providers possess distinct yet complementary roles in stroke prevention. Physicians focus on managing cardiovascular risk factors such as hypertension, diabetes, and hyperlipidemia, often prescribing medications and monitoring vital signs. They may also conduct neurological examinations to detect early signs of stroke. In contrast, oral health professionals assess oral health, identify periodontal disease, and provide preventive and therapeutic interventions. The early detection of periodontal disease, a known risk factor for stroke, is a key contribution made by dental professionals. This collaborative approach allows for a holistic assessment of a patient’s health, maximizing the effectiveness of preventive measures.
Roles in Stroke Prevention: A Comparative Analysis
Oral health professionals primarily focus on identifying and managing oral health conditions, particularly periodontal disease, which has been linked to an increased risk of stroke. Their contributions include conducting thorough oral examinations, identifying signs of periodontal inflammation, and educating patients on oral hygiene practices. Physicians, on the other hand, concentrate on managing systemic risk factors for stroke, such as hypertension and diabetes, through medication management and lifestyle modifications. They also play a crucial role in diagnosing and treating stroke when it occurs. Registered nurses and other healthcare professionals assist with patient education, medication adherence, and monitoring for potential stroke symptoms. This division of labor, while distinct, is highly interdependent, with each professional’s expertise contributing to a comprehensive approach to stroke prevention.
Effective Communication: Improving Patient Outcomes
Effective communication between dental professionals and physicians is paramount in improving patient outcomes. For instance, a dentist discovering severe periodontal disease in a patient should promptly communicate this finding to the patient’s physician. This allows for a joint assessment of cardiovascular risk, facilitating timely interventions to mitigate the increased risk of stroke. Conversely, a physician aware of a patient’s history of stroke or cardiovascular disease should inform the dental professional, enabling the dentist to adjust treatment plans accordingly and minimize potential risks during dental procedures. This communication can be facilitated through secure electronic health records, direct referrals, or collaborative care models. Clear, concise communication, including shared clinical notes and relevant test results, is vital for successful interprofessional collaboration.
Model for Interprofessional Collaboration
A successful model for interprofessional collaboration in stroke prevention could involve the establishment of a shared care pathway. This pathway would define clear roles and responsibilities for each healthcare professional involved in a patient’s care, outlining communication protocols and decision-making processes. Regular meetings between oral health professionals and physicians could be incorporated into this model to discuss patient cases, share information, and coordinate care. This shared care pathway should be integrated into existing healthcare systems, utilizing electronic health records to facilitate information sharing and tracking of patient progress. The pathway should also incorporate patient education materials, promoting patient empowerment and engagement in their own health management. A multidisciplinary team, comprising physicians, dentists, nurses, and other relevant healthcare professionals, could manage and monitor the implementation of this shared care pathway, ensuring its effectiveness and ongoing improvement.
Integrating Oral Health Screenings into Stroke Prevention Programs
Integrating oral health screenings into existing stroke prevention programs can be achieved by incorporating oral health assessments into routine check-ups. This could involve adding a simple periodontal screening, including measuring gingival inflammation and probing pocket depths, to existing cardiovascular risk assessments. The results of these screenings would then be shared with the patient’s physician, allowing for a more comprehensive risk stratification and appropriate interventions. Training existing healthcare professionals in basic oral health assessment techniques can facilitate this integration. Public health campaigns emphasizing the link between oral health and stroke risk could also be implemented to raise public awareness and encourage participation in both oral health and cardiovascular health screenings. This integrated approach provides a cost-effective and efficient way to enhance stroke prevention efforts.
Illustrative Case Studies

This section presents hypothetical case studies to illustrate the connection between oral health and stroke risk, highlighting the impact of oral health interventions on cardiovascular health outcomes. These examples are intended to be representative of real-world scenarios and emphasize the importance of proactive oral health care.
Case Study 1: The Impact of Poor Oral Health on Stroke Risk
Mr. Jones, a 65-year-old male with a history of poorly controlled diabetes and hypertension, presented with severe periodontal disease characterized by significant gum inflammation, bleeding, and tooth loss. He reported infrequent dental visits and neglected his oral hygiene. His blood tests revealed elevated levels of C-reactive protein (CRP), a marker of inflammation. Furthermore, his echocardiogram showed subtle signs of left ventricular hypertrophy, a condition often associated with hypertension and increased stroke risk. The combination of uncontrolled systemic inflammation stemming from his periodontal disease, coupled with his existing cardiovascular risk factors, significantly increased his likelihood of experiencing a stroke. His case underscores the systemic impact of periodontal disease and its contribution to overall cardiovascular health.
Case Study 2: Positive Impact of Oral Health Intervention
Ms. Smith, a 70-year-old female with a history of hypertension, underwent a comprehensive oral health assessment that revealed moderate periodontal disease. Following a detailed explanation of the link between oral health and cardiovascular health, she committed to improved oral hygiene practices, including regular brushing, flossing, and the use of an antimicrobial mouthwash. She also began attending regular dental check-ups for professional cleaning and periodontal treatment. Within six months, her gingival inflammation significantly reduced, and her CRP levels decreased. Her subsequent echocardiogram showed improvement in her left ventricular hypertrophy. This case demonstrates how targeted oral health interventions can positively impact systemic inflammation and potentially reduce the risk of cardiovascular events like stroke.
Case Study 3: Improved Oral Healthcare Contributing to a Positive Outcome
Mrs. Garcia, a 58-year-old female, presented with early signs of periodontal disease and a family history of stroke. Proactive intervention, including regular professional cleanings, periodontal therapy, and education on optimal oral hygiene, was implemented. Her regular dental checkups allowed for early detection and management of periodontal disease, preventing further progression and reducing systemic inflammation. This preventative approach, combined with her adherence to a healthy lifestyle, contributed to a significantly reduced risk of stroke compared to individuals with similar risk profiles who did not receive comparable oral healthcare.
Case Study 4: Negative Outcome Due to Lack of Access to Oral Healthcare
Mr. Rodriguez, a 62-year-old male with a history of uncontrolled hypertension and diabetes, lacked access to regular dental care due to financial constraints and geographical limitations. His advanced periodontal disease went untreated, leading to persistent systemic inflammation. He experienced a significant stroke, and the severity of the stroke was potentially exacerbated by the chronic inflammation associated with his untreated periodontal disease. This case highlights the critical role of equitable access to oral healthcare in preventing adverse cardiovascular outcomes, emphasizing the need for community-based programs and initiatives that address healthcare disparities.

Tim Redaksi