Defining Health Informatics Ethics: Do Health Informatics Have A Wrirten Code Of Ethics
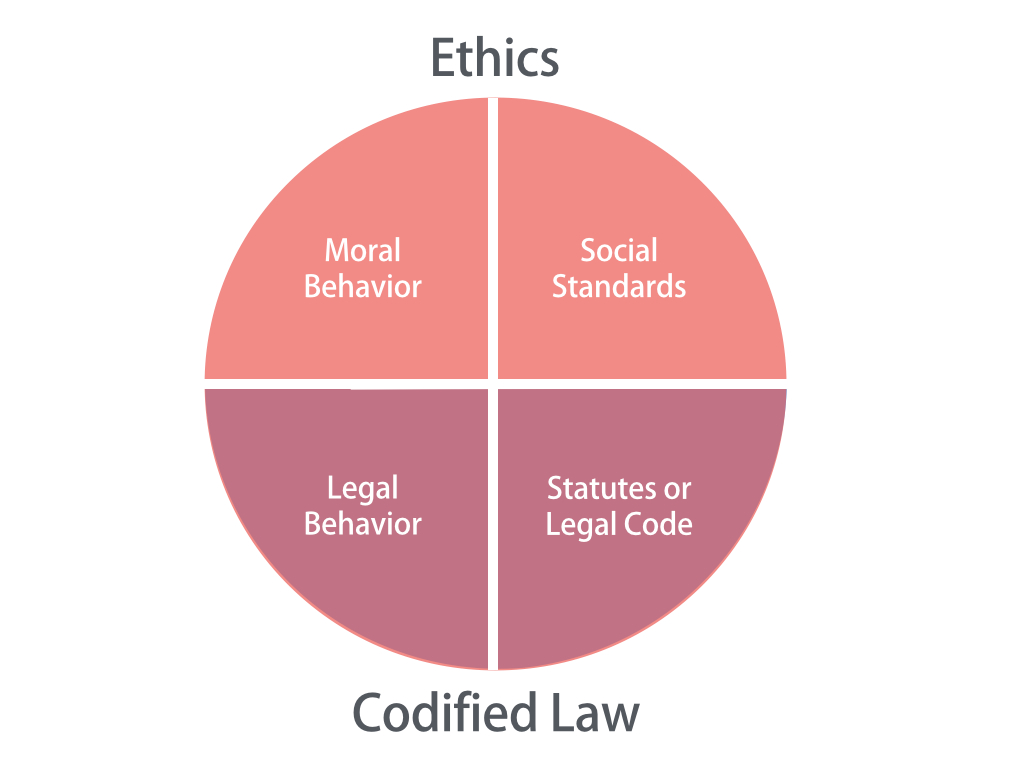
Health informatics ethics concerns the moral principles and values governing the responsible development, implementation, and use of health information technologies and systems. It’s a complex field navigating the intersection of technological advancements, patient rights, data security, and the overall goal of improving healthcare. This involves considering the impact of these technologies on individuals, healthcare organizations, and society as a whole.
Health informatics ethics builds upon core principles generally accepted in professional ethics, adapting them to the unique challenges presented by the digital healthcare landscape. These core principles typically include beneficence (acting in the best interests of patients), non-maleficence (avoiding harm), respect for autonomy (respecting patient choices and self-determination), justice (fair and equitable distribution of resources and benefits), and fidelity (maintaining trust and loyalty). However, the application of these principles in health informatics often requires nuanced interpretations and careful consideration of potential conflicts.
Ethical Dilemmas in Health Informatics
Several ethical dilemmas are unique to health informatics. One significant challenge involves balancing patient privacy and data security with the need for data sharing to improve research and care coordination. For example, the use of electronic health records (EHRs) allows for efficient data access, but also raises concerns about unauthorized access, data breaches, and the potential for misuse of sensitive patient information. Another dilemma arises from the development and deployment of artificial intelligence (AI) in healthcare. While AI algorithms can potentially improve diagnostic accuracy and treatment planning, concerns exist about algorithmic bias, lack of transparency in decision-making processes, and the potential for displacement of human healthcare professionals. The development and use of telehealth platforms also present ethical considerations regarding patient access, quality of care, and the potential for widening existing health disparities. Finally, the increasing use of wearable health trackers and other consumer health technologies raises questions about data ownership, informed consent, and the potential for misuse of personal health data by commercial entities.
Comparison with Related Fields
Health informatics ethics shares overlaps with, yet also differs from, the ethics of related fields like medicine and computer science. It shares with medical ethics a strong emphasis on patient well-being, beneficence, and non-maleficence. However, health informatics also incorporates considerations specific to technology, such as data security, algorithmic fairness, and the impact of automation on healthcare workflows. Compared to computer science ethics, health informatics places a greater emphasis on the human element and the potential impact of technology on vulnerable populations. While computer science ethics often focuses on issues such as software security, intellectual property, and the societal impact of technology in general, health informatics ethics narrows this focus to the specific context of healthcare, emphasizing the ethical implications for patients and healthcare providers. For instance, a computer scientist might focus on the security vulnerabilities of a particular algorithm, while a health informatician would also consider the potential consequences of a security breach on patient privacy and the trust between patients and healthcare providers.
Key Ethical Issues in Health Informatics Practice
Health informatics, while offering immense potential for improving healthcare, presents several complex ethical challenges. The increasing reliance on technology to store, manage, and analyze patient data necessitates a robust ethical framework to guide practitioners and ensure responsible innovation. This section will explore some key ethical issues arising from the practice of health informatics.
Data Privacy and Security in Health Informatics
The ethical implications of data privacy and security are paramount in health informatics. Health information is highly sensitive, containing details about individuals’ physical and mental health, genetic predispositions, and lifestyle choices. Unauthorized access, disclosure, or modification of this data can have severe consequences, including reputational damage, discrimination, and even physical harm. The potential for breaches is amplified by the interconnected nature of modern health IT systems, increasing the risk of large-scale data leaks. Strong security measures, including encryption, access controls, and regular audits, are crucial. Furthermore, adherence to regulations like HIPAA in the United States and GDPR in Europe is vital to maintaining patient trust and ensuring legal compliance. The ethical responsibility extends beyond technical safeguards; it also includes educating healthcare professionals and patients about data privacy risks and best practices. Failure to prioritize data security not only violates ethical principles but also erodes public confidence in the use of health information technology.
Conflict Between Patient Autonomy and Efficient Use of Health Information Technology, Do health informatics have a wrirten code of ethics
Consider a scenario where a hospital implements a new electronic health record (EHR) system designed to improve efficiency and reduce medical errors. The system allows for the automated sharing of patient data across different departments and healthcare providers. However, a patient, Mr. Jones, explicitly requests that his allergy information not be shared with certain specialists due to a past negative experience. The efficient functioning of the EHR system, however, relies on the seamless flow of all relevant patient data. This creates a conflict: respecting Mr. Jones’ autonomy and right to control his information versus maximizing the efficiency and potential benefits of the new technology for all patients. Resolving this requires careful consideration of the potential risks and benefits to both the individual and the broader healthcare system. Balancing patient autonomy with the overall goal of improving healthcare quality and efficiency requires thoughtful design of health IT systems and clear communication with patients about data sharing practices.
Approaches to Resolving Ethical Conflicts in Health Informatics
The resolution of ethical conflicts in health informatics often requires a multi-faceted approach. Different stakeholders will hold varying perspectives, and the chosen solution must carefully balance competing interests.
| Ethical Issue | Stakeholder Perspectives | Potential Solutions | Outcomes |
|---|---|---|---|
| Data Breach Affecting Patient Privacy | Patients: fear of identity theft, discrimination; Healthcare providers: concern about legal liability; IT professionals: responsibility for system security | Implement robust security measures, transparent communication with affected patients, comprehensive breach response plan, and legal counsel | Minimized reputational damage, maintained patient trust, and compliance with legal requirements. |
| Conflicting patient preferences regarding data sharing | Patient: desire for control over personal data; Clinicians: need for comprehensive information for optimal care; Hospital administration: desire for efficient data flow | Develop clear policies on data sharing with opt-in/opt-out options; Provide patients with education on data privacy and security; Implement granular access controls within the EHR system | Improved patient engagement, enhanced clinical decision-making, and strengthened trust between patients and healthcare providers. |
| Algorithmic bias in clinical decision support systems | Patients: concern about fairness and equity; Clinicians: need for reliable and unbiased tools; Developers: responsibility for algorithm design and testing | Rigorous algorithm testing and validation; diverse datasets for training; ongoing monitoring for bias; transparent communication with patients and clinicians | More equitable healthcare outcomes, improved trust in technology, and greater accountability in algorithm development. |
| Access to healthcare information for underserved populations | Patients: need for equitable access; Healthcare providers: challenges in reaching remote or disadvantaged communities; Policymakers: responsibility for resource allocation | Telehealth initiatives, mobile health applications, culturally competent health information resources, and community outreach programs | Improved health equity, increased access to care, and reduced health disparities. |

Tim Redaksi