Influence on Patient-Provider Relationship
Background assumptions significantly shape the dynamics of the patient-provider relationship, impacting communication, trust, and the overall effectiveness of care. These assumptions, often unconscious, can create barriers to understanding and lead to misinterpretations, hindering the therapeutic alliance. Understanding how these assumptions operate is crucial for fostering more equitable and effective healthcare interactions.
How do background assumptions affect behavioral health – Differing background assumptions can manifest as significant communication barriers in the patient-provider relationship. For example, a provider from a predominantly individualistic culture might assume a patient’s reluctance to share family details stems from a lack of trust, while the patient, from a collectivist culture, might prioritize family privacy and view the question as intrusive. Similarly, differing understandings of time, personal space, and even the expression of emotions can lead to misunderstandings and frustration. These misinterpretations can range from minor inconveniences to major breakdowns in communication, impacting treatment adherence and overall health outcomes.
Communication Strategies Addressing Diverse Background Assumptions
Effective communication strategies acknowledge and actively address the potential influence of diverse background assumptions. This involves employing culturally sensitive communication techniques, such as active listening, reflective questioning, and careful attention to nonverbal cues. Providers should strive to create a safe space for patients to share their perspectives and experiences without judgment. Furthermore, utilizing interpreters when necessary and being mindful of language barriers are critical. A key component is demonstrating empathy and understanding, actively seeking clarification to avoid misinterpretations. For example, instead of assuming a patient’s silence indicates agreement, the provider might ask, “Can you tell me more about what you’re thinking?” or “Is there anything else you’d like to share?”. These strategies help bridge cultural gaps and foster a more equitable therapeutic relationship.
Impact of Assumptions on Trust and Rapport
Assumptions significantly impact the development of trust and rapport between patients and providers. When providers make inaccurate assumptions about a patient’s background, beliefs, or experiences, it can erode trust and create a sense of being misunderstood or dismissed. This is particularly true for patients from marginalized communities who may have experienced discrimination or bias within healthcare settings. Conversely, when providers demonstrate cultural sensitivity and actively challenge their own assumptions, it fosters a sense of safety, respect, and trust, strengthening the therapeutic alliance and improving treatment outcomes. Building rapport requires genuine effort to understand the patient’s unique perspective and create a collaborative partnership.
Strategies for Providers to Actively Challenge Their Own Background Assumptions
Providers can proactively challenge their own background assumptions through various strategies. Regular reflection on personal biases and assumptions is essential. This can involve self-assessment tools, participation in cultural competency training, and seeking feedback from colleagues and supervisors. Engaging in continuous learning about diverse cultures and healthcare experiences broadens understanding and reduces reliance on stereotypes. Furthermore, actively seeking out diverse perspectives through mentorship, collaboration with community organizations, and seeking patient feedback helps challenge preconceived notions and cultivate a more inclusive approach to care. Seeking supervision or consultation when encountering challenges related to cultural differences allows for a more informed and nuanced approach to patient care.
The Role of Systemic Factors: How Do Background Assumptions Affect Behavioral Health
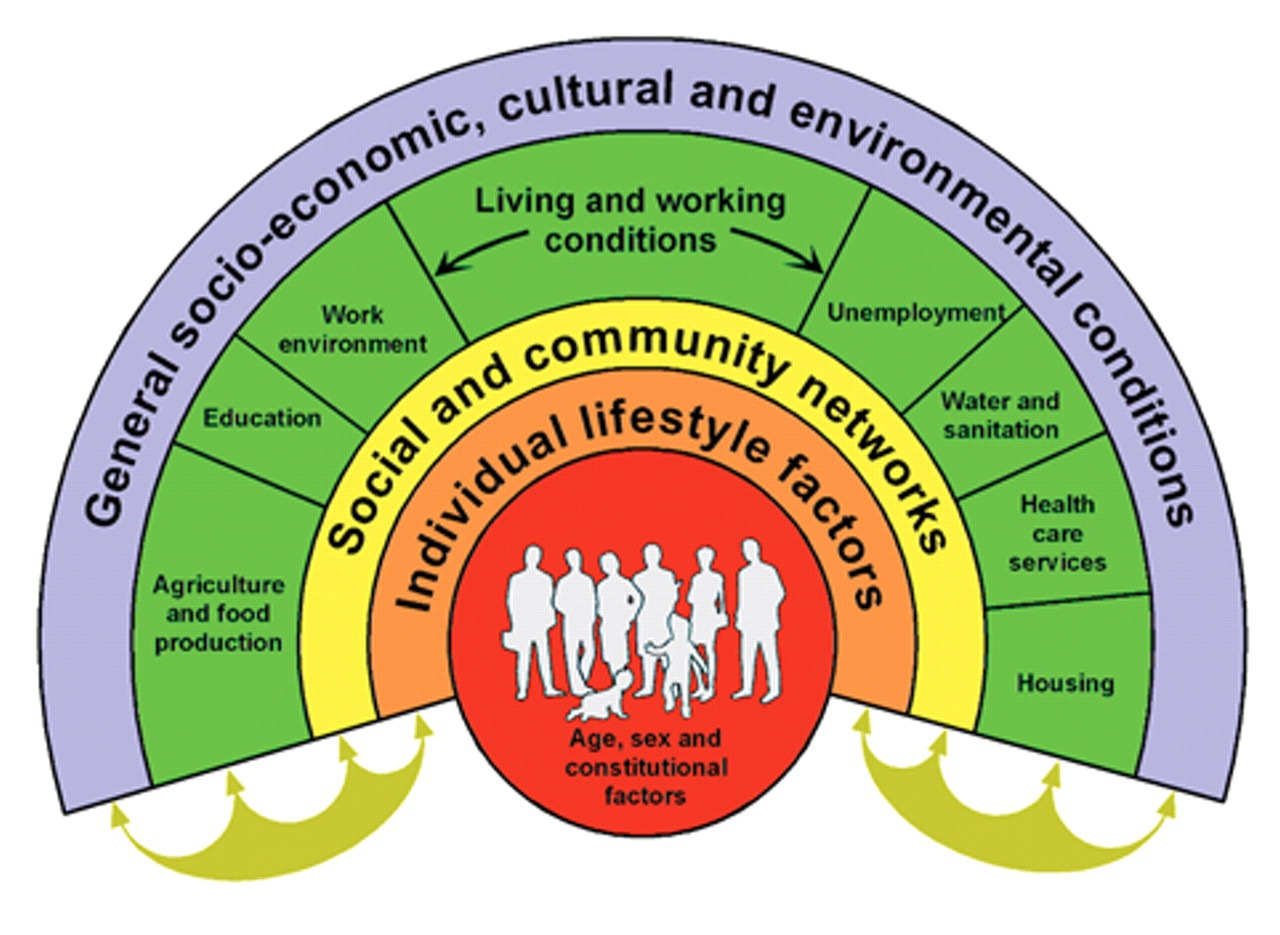
Societal and institutional biases significantly impact access to and outcomes within behavioral healthcare. These systemic factors create and perpetuate disparities, influencing not only who receives care but also the quality and effectiveness of that care. Understanding these influences is crucial for developing equitable and effective interventions.
Systemic factors, deeply embedded within the structures of our societies and institutions, create a complex web of influence on background assumptions in behavioral health. These assumptions, often unconscious, shape perceptions of patients, treatment approaches, and resource allocation. The resulting disparities are not simply the result of individual prejudice but rather the product of broader societal and institutional structures.
Societal and Institutional Biases and Healthcare Disparities
Societal biases, such as racism, sexism, homophobia, and classism, manifest in healthcare through unequal access to resources, discriminatory practices, and biased diagnostic criteria. For instance, individuals from marginalized communities may face greater difficulty accessing mental health services due to financial barriers, geographical limitations, or lack of culturally competent providers. This limited access can lead to delayed or inadequate treatment, resulting in poorer outcomes. Institutional biases, reflected in policies and procedures within healthcare systems, further exacerbate these inequalities. These biases can manifest in the form of unequal resource allocation, discriminatory hiring practices, or the perpetuation of stereotypes within clinical settings. For example, a hospital system prioritizing affluent neighborhoods over underserved areas inherently creates a disparity in access to care.
Systemic Factors and the Perpetuation of Harmful Background Assumptions
Systemic factors contribute to the persistence of harmful background assumptions by reinforcing existing power structures and social norms. For example, the overrepresentation of certain diagnostic categories in specific populations may reflect biased assessment practices rather than actual prevalence rates. Similarly, a lack of diversity among healthcare professionals can lead to misinterpretations of cultural expressions and behaviors, resulting in misdiagnosis or inappropriate treatment. These patterns are self-perpetuating; biased assumptions shape clinical practices, which in turn reinforce those same assumptions.
Examples of Policies and Practices Reinforcing Biased Assumptions
Several policies and practices unintentionally, or sometimes intentionally, reinforce biased assumptions in behavioral health settings. One example is the disproportionate use of involuntary commitment for individuals from marginalized communities. Another is the underfunding of community-based mental health services in underserved areas, forcing individuals to rely on emergency rooms or jails for care. Additionally, diagnostic criteria may be culturally insensitive, leading to misdiagnosis and inappropriate treatment for individuals from diverse cultural backgrounds. The lack of interpreter services for patients with limited English proficiency can also create significant barriers to care and lead to miscommunication and misunderstanding.
Designing Interventions to Mitigate the Impact of Systemic Factors
Addressing the impact of systemic factors requires multifaceted interventions targeting both individual biases and institutional structures. These interventions should focus on increasing cultural competency among healthcare providers, improving access to care for marginalized communities, and promoting equitable resource allocation. Examples include implementing culturally sensitive training programs for healthcare professionals, expanding access to telehealth services in underserved areas, and developing culturally adapted diagnostic tools. Furthermore, policies promoting diversity and inclusion within healthcare systems, alongside the implementation of robust data collection and analysis to monitor disparities, are essential for creating a more equitable behavioral healthcare system. Finally, investing in community-based mental health services and promoting collaborative partnerships between healthcare providers and community organizations can significantly improve access to and quality of care for all individuals.
Ethical Considerations

The influence of background assumptions on behavioral health presents several complex ethical dilemmas that require careful consideration. Failing to acknowledge and address these biases can lead to misdiagnosis, ineffective treatment, and the perpetuation of health disparities. Ethical practice demands a proactive approach to understanding and mitigating the impact of personal and societal biases on patient care.
Ethical dilemmas arising from the influence of background assumptions are multifaceted and can significantly impact the quality and equity of care. For instance, a provider’s implicit biases regarding race, socioeconomic status, or gender identity might lead to misinterpretations of patient behavior, resulting in inaccurate diagnoses or inappropriate treatment plans. Similarly, assumptions about a patient’s cultural background might lead to a lack of cultural sensitivity, hindering effective communication and trust-building. The potential for harm is substantial, highlighting the critical need for ethical reflection and responsible practice.
Cultural Competence and Sensitivity in Ethical Care, How do background assumptions affect behavioral health
Cultural competence is not merely a matter of politeness; it is a fundamental ethical requirement in behavioral health. It involves actively seeking to understand the patient’s unique cultural context, including their beliefs, values, and practices, and adapting treatment approaches accordingly. This requires ongoing learning, self-reflection, and a commitment to humility in the face of diverse perspectives. Providers must actively avoid imposing their own cultural frameworks onto patients and instead strive to create a therapeutic relationship built on mutual respect and understanding. For example, a therapist working with a patient from a collectivist culture should be mindful of the importance of family involvement in decision-making, rather than assuming individual autonomy as the primary focus. Ignoring these cultural nuances can lead to ineffective therapy and damage the therapeutic alliance.
Addressing Personal Biases and Assumptions
Healthcare providers have a professional responsibility to engage in ongoing self-reflection and critical self-assessment to identify and address their own biases and assumptions. This is not a one-time task, but rather an ongoing process of learning and growth. Strategies for addressing personal biases include seeking supervision and consultation, participating in continuing education on cultural competence and diversity, and engaging in regular self-reflection exercises. For instance, journaling about potential biases encountered during patient interactions can be a powerful tool for increased awareness. The goal is not to eliminate all biases—that is an unrealistic expectation—but rather to become aware of their potential influence and to mitigate their impact on clinical judgment and patient care. Ignoring personal biases demonstrates a lack of professional responsibility and can lead to significant harm for patients.
Best Practices for Ethical Decision-Making
Ethical decision-making in the context of background assumptions requires a systematic and reflective approach. The following best practices can help guide providers:
Several strategies are crucial for navigating ethical dilemmas stemming from background assumptions. These strategies emphasize proactive self-reflection, continuous learning, and a commitment to patient-centered care.
- Regular Self-Reflection: Journaling, supervision, and peer consultation are essential tools for identifying and addressing personal biases.
- Cultural Humility: Recognize the limitations of one’s own cultural understanding and approach each patient with openness and a willingness to learn.
- Seeking Consultation: Don’t hesitate to consult with colleagues, supervisors, or ethics committees when faced with complex ethical dilemmas.
- Evidence-Based Practice: Ground clinical decisions in evidence-based research, minimizing the influence of personal biases.
- Patient-Centered Care: Prioritize the patient’s values, preferences, and cultural context in all aspects of care.

Tim Redaksi