Information Gathering Methods in Healthcare: What Does Help Gather Information Look Like For Health

Effective information gathering is paramount in healthcare, forming the bedrock of accurate diagnoses, appropriate treatment plans, and positive patient outcomes. The process involves a multifaceted approach, utilizing various methods to obtain a comprehensive understanding of the patient’s health status. This includes not only the present condition but also their medical history and lifestyle factors.
Methods of Gathering Patient Information
Healthcare professionals employ a range of methods to collect patient information. These methods are often used in combination to provide a holistic view of the patient’s health. The following table summarizes key methods, their strengths, and weaknesses.
| Method | Description | Strengths | Weaknesses |
|---|---|---|---|
| Patient Interview | A structured or unstructured conversation between the healthcare provider and the patient to gather information about their symptoms, medical history, lifestyle, and concerns. | Allows for open-ended exploration of patient concerns; builds rapport; gathers subjective data directly from the patient. | Can be time-consuming; prone to recall bias; subjective information may be incomplete or inaccurate; patient may be reluctant to disclose sensitive information. |
| Physical Examination | A systematic assessment of the patient’s body, including vital signs, auscultation, palpation, and percussion, to detect physical abnormalities. | Provides objective data; allows for immediate assessment of physical condition; can detect subtle signs and symptoms. | Requires specialized training and skill; may be uncomfortable or invasive for some patients; some conditions may not be detectable through physical examination alone. |
| Review of Medical Records | Examination of previous medical records, including lab results, imaging reports, and previous treatment plans. | Provides a comprehensive overview of the patient’s medical history; allows for identification of trends and patterns; avoids repetition of tests. | Records may be incomplete or inaccurate; access to records may be limited; information may be outdated. |
| Diagnostic Testing | Utilizing various tests such as blood tests, imaging studies (X-rays, CT scans, MRI), and biopsies to obtain objective data about the patient’s condition. | Provides objective and quantifiable data; can confirm or rule out diagnoses; aids in treatment planning. | Can be expensive and time-consuming; some tests carry risks; results may not always be conclusive. |
Structured versus Unstructured Data Collection
Structured data collection involves using standardized forms and templates to gather information, ensuring consistency and ease of analysis. Unstructured data collection, on the other hand, involves collecting information in a free-flowing format, such as through open-ended interviews or narrative notes. Structured data is more readily analyzed using computational methods, leading to more efficient data management and the potential for large-scale research. However, unstructured data often provides richer qualitative information, offering valuable insights that may be missed with a structured approach. The ideal approach often involves a combination of both methods to maximize the benefits of each. For example, a structured questionnaire about symptoms might be followed by an unstructured interview to explore the patient’s experience in more detail.
Ethical Considerations in Gathering Sensitive Patient Information
Gathering sensitive patient information necessitates strict adherence to ethical guidelines. This includes obtaining informed consent, ensuring confidentiality through HIPAA compliance (in the US) or equivalent regulations in other countries, and protecting patient privacy. Healthcare professionals must be mindful of the potential for bias and discrimination and ensure that data collection practices do not perpetuate inequalities. Data security is paramount, requiring robust measures to prevent unauthorized access and data breaches. Transparency about how data is used and shared is crucial to building trust with patients. For instance, patients should be clearly informed about how their data will be used for research purposes and have the right to opt out.
Role of Technology in Information Gathering
Technology has revolutionized healthcare information gathering, moving from paper-based systems to sophisticated digital platforms that enhance efficiency, accuracy, and accessibility of patient data. This transformation has significantly improved the quality of care and enabled proactive health management.
Electronic health records (EHRs) and other health information technologies are fundamental to this progress. They provide a centralized repository for a patient’s complete medical history, facilitating seamless information sharing among healthcare providers. This reduces redundancy, minimizes errors associated with manual record-keeping, and enables better-informed decision-making.
Electronic Health Records and Health Information Technologies
EHRs integrate various aspects of patient care, including diagnoses, medications, allergies, immunization records, lab results, and imaging reports. This comprehensive view allows clinicians to quickly access critical information, leading to faster diagnoses, more effective treatment plans, and reduced healthcare costs. Other health information technologies, such as hospital information systems (HIS) and practice management software, further streamline administrative tasks and improve workflow efficiency within healthcare settings. For example, HIS systems manage patient admissions, discharges, and transfers, while practice management software assists with billing, scheduling, and communication with patients. The integration of these systems ensures that all relevant information is readily available to the appropriate personnel at the right time.
Wearable Health Trackers and Remote Monitoring Devices
Wearable health trackers and remote monitoring devices represent a significant advancement in data collection, enabling continuous monitoring of vital signs and other health parameters outside of traditional clinical settings. These devices, such as smartwatches and fitness trackers, can collect data on heart rate, activity levels, sleep patterns, and even blood glucose levels. Remote monitoring devices, often used for patients with chronic conditions, transmit physiological data directly to healthcare providers, allowing for early detection of potential problems and timely intervention. For instance, a patient with congestive heart failure might use a remote monitoring device to transmit their weight and blood pressure readings daily, enabling proactive management of their condition and preventing hospital readmissions.
Artificial Intelligence in Health Information Analysis
Artificial intelligence (AI) offers immense potential for analyzing large volumes of health information, identifying patterns, and making predictions that can improve patient outcomes. AI algorithms can analyze EHR data to identify patients at risk of developing certain conditions, predict adverse drug reactions, and personalize treatment plans. For example, AI can analyze medical images to detect cancerous lesions earlier and more accurately than human radiologists alone. However, the effective use of AI requires careful consideration of data quality, algorithm bias, and ethical implications.
Potential Biases Introduced by Technology in Health Data Gathering
The use of technology in health data gathering, while offering significant advantages, can also introduce biases that may affect the accuracy and fairness of healthcare services. It is crucial to be aware of these potential biases to mitigate their impact.
- Selection Bias: Technology access disparities can lead to biased data representation, where certain populations with limited access to technology are underrepresented.
- Algorithm Bias: AI algorithms trained on biased data can perpetuate and amplify existing health disparities. For instance, an algorithm trained primarily on data from one demographic group may not perform as well for other groups.
- Measurement Bias: Wearable devices may not accurately capture data for all individuals, particularly those with diverse body types or activity levels. This can lead to inaccurate assessments of health status.
- Data Privacy and Security Concerns: The collection and storage of sensitive health data through technology raise concerns about data breaches and unauthorized access.
- Reporting Bias: Patients may selectively report data based on social desirability or other factors, leading to inaccuracies in self-reported data from wearable devices or online questionnaires.
Patient Involvement in Information Gathering
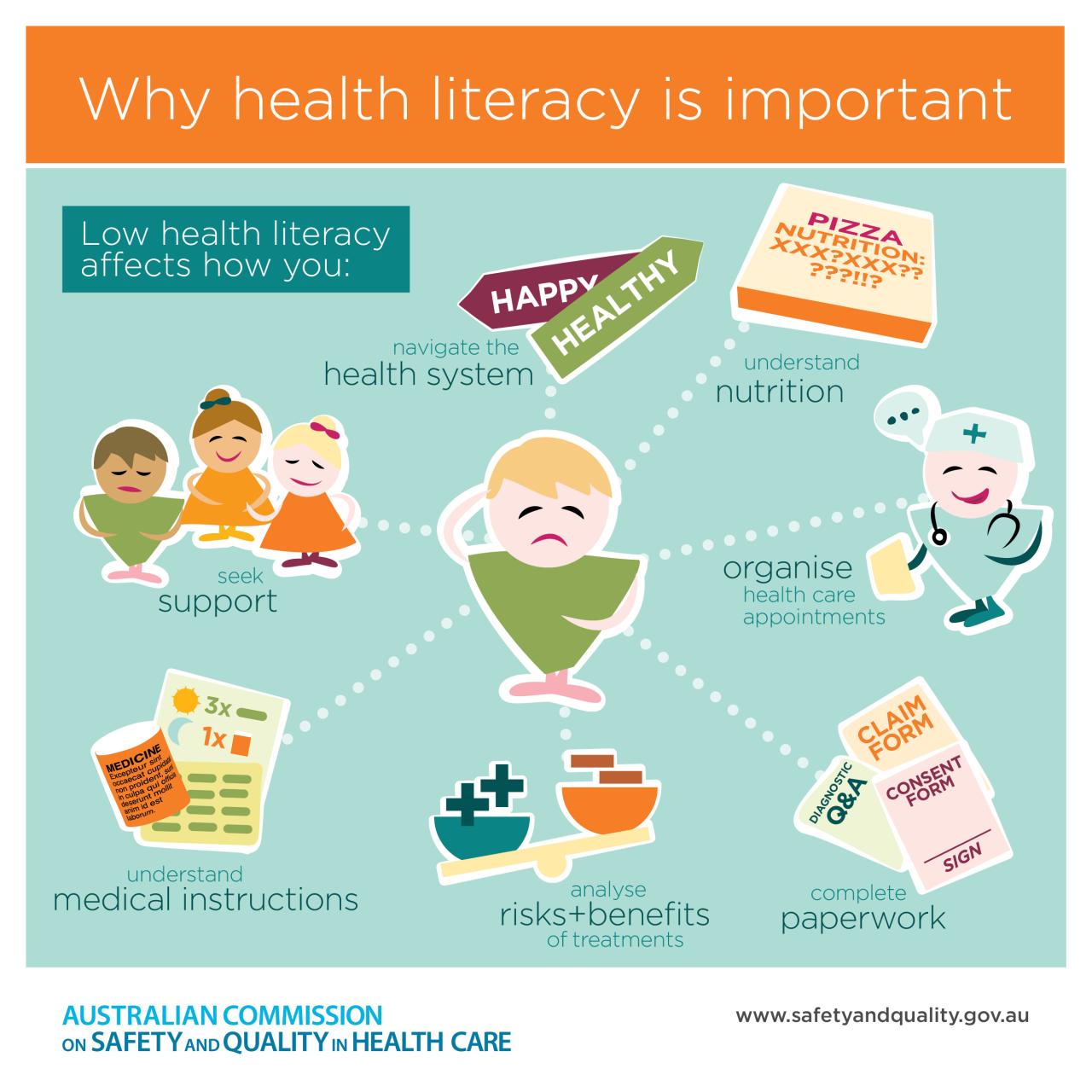
Accurate and complete health information is the cornerstone of effective healthcare. Patients are the primary source of much of this information, possessing unique insights into their own bodies, lifestyles, and medical histories that healthcare providers simply cannot access otherwise. Their active participation is therefore crucial for delivering the best possible care and achieving optimal health outcomes. Engaging patients effectively in the information gathering process not only improves the quality of care but also fosters a stronger doctor-patient relationship built on trust and collaboration.
Effective communication is paramount when gathering health information from patients. A sensitive and empathetic approach is essential to create a safe space for open dialogue. Providers should actively listen to patients, ask clear and concise questions, and avoid using medical jargon that may be confusing or intimidating. Furthermore, employing techniques like motivational interviewing can encourage patients to reflect on their health behaviors and provide more comprehensive information. Visual aids, such as diagrams or charts, can also aid in understanding complex medical concepts and facilitating clear communication. Summarizing key points throughout the conversation helps ensure mutual understanding and avoids misunderstandings. Finally, respecting patient confidentiality and ensuring data privacy builds trust and encourages open communication.
Strategies for Effective Patient Communication, What does help gather information look like for health
Effective communication techniques are crucial for eliciting accurate and complete health information from patients. Employing active listening skills, such as paying close attention to both verbal and nonverbal cues, allows healthcare providers to fully understand the patient’s perspective. Using open-ended questions, such as “Can you tell me more about your symptoms?” encourages detailed responses, while closed-ended questions, such as “Do you experience chest pain?”, are useful for confirming specific information. The use of plain language, avoiding medical jargon, is vital to ensure clear understanding. Regularly summarizing the patient’s responses helps confirm accuracy and allows for clarification. Providing opportunities for patients to ask questions fosters a collaborative relationship and encourages open communication. Finally, creating a comfortable and non-judgmental environment ensures patients feel safe sharing sensitive information. For example, a provider might start a conversation by saying, “I understand this can be a difficult conversation, and I want to assure you that I’m here to listen without judgment.”
Patient Questionnaire for Comprehensive Health Information
A well-designed questionnaire can efficiently gather comprehensive health information. The questionnaire should be structured clearly, using simple language and avoiding overly technical terms. It should cover key aspects of a patient’s lifestyle, medical history, and current health concerns, while respecting patient privacy. Information gathered should be used responsibly and ethically, adhering to all relevant privacy regulations.
- Demographic Information: Name, age, gender, contact information, and date of birth.
- Lifestyle Factors: Smoking status (current smoker, former smoker, never smoked), alcohol consumption (frequency and amount), physical activity level (frequency, duration, and type), diet (general description), sleep habits (hours of sleep per night, sleep quality).
- Medical History: Past illnesses, hospitalizations, surgeries, allergies (medications, foods, environmental factors), current medications (prescription and over-the-counter), family history of diseases (cancer, heart disease, diabetes, etc.).
- Current Health Concerns: Description of current symptoms (onset, duration, severity, location), any recent changes in health status, concerns about specific body systems (e.g., respiratory, cardiovascular, gastrointestinal).
- Mental Health: Any history of mental health conditions (depression, anxiety, etc.), current mental health status, stress levels.
- Social History: Marital status, occupation, living situation, social support network.
- Environmental Factors: Exposure to environmental toxins (e.g., asbestos, lead), living conditions (e.g., housing quality, access to clean water).
Data Security and Privacy in Health Information Gathering
The collection and use of patient health information necessitate robust security and privacy measures. Failure to protect this sensitive data can lead to legal repercussions, reputational damage, and significant harm to patients. This section Artikels the legal and ethical obligations surrounding patient data, explores practical security measures, and examines the consequences of data breaches.
What does help gather information look like for health – Legal and ethical requirements for protecting patient health information are multifaceted and vary by jurisdiction. However, several core principles consistently apply. These include the obligation to maintain confidentiality, the need for informed consent regarding data use, and the responsibility to ensure data integrity and availability. Specific regulations, such as HIPAA in the United States and GDPR in the European Union, provide detailed guidelines and penalties for non-compliance. Ethical considerations extend beyond legal mandates, encompassing principles of respect for autonomy, beneficence, and non-maleficence in the handling of patient data.
Legal and Ethical Requirements for Protecting Patient Health Information
Healthcare providers must adhere to a complex framework of laws and ethical guidelines to protect patient health information. Key regulations like HIPAA (Health Insurance Portability and Accountability Act) in the United States and GDPR (General Data Protection Regulation) in the European Union establish stringent requirements for data security, patient consent, and data breach notification. These regulations define protected health information (PHI), outlining what data is considered sensitive and requiring specific safeguards for its handling. Ethical principles, such as patient autonomy (respecting a patient’s right to control their information), beneficence (acting in the patient’s best interest), and non-maleficence (avoiding harm), guide the responsible and ethical use of patient data, even beyond the strict letter of the law.
Measures to Ensure Confidentiality and Security of Collected Data
Implementing robust security measures is crucial to safeguarding patient data. This includes utilizing strong encryption methods for data both in transit and at rest, implementing strict access control protocols (limiting access to authorized personnel only, based on the principle of least privilege), and regularly conducting security audits and vulnerability assessments. Employee training on data security best practices is also essential. Physical security measures, such as secure storage of physical files and controlled access to facilities, are equally important. Furthermore, data minimization—collecting only the necessary data—reduces the potential impact of a breach. Regular backups and disaster recovery plans ensure data availability even in the event of a system failure or cyberattack.
Implications of Data Breaches in the Healthcare Context
Data breaches in healthcare have far-reaching consequences. The unauthorized disclosure of patient health information can lead to identity theft, financial fraud, and reputational damage for the healthcare provider. Patients may experience emotional distress, loss of trust in the healthcare system, and potential discrimination. Financially, data breaches can result in significant fines and legal costs for the organization. In addition, the reputational harm can affect patient acquisition and retention. For example, a large hospital system experiencing a data breach resulting in the exposure of thousands of patients’ medical records might face substantial legal penalties, loss of public trust, and a decline in new patients.
Secure Storage and Access of Patient Health Information
A secure process for storing and accessing patient health information is critical. This process should incorporate several key steps, from data collection to secure disposal.
The following flowchart illustrates a simplified process:
Flowchart: Secure Storage and Access of Patient Health Information
1. Data Collection: Patient data is collected using secure methods (e.g., encrypted forms, secure portals).
2. Data Entry: Data is entered into a secure electronic health record (EHR) system with access controls.
3. Data Storage: Data is stored on encrypted servers with regular backups and disaster recovery plans in place.
4. Data Access: Access is granted only to authorized personnel with appropriate credentials, using multi-factor authentication.
5. Data Use: Data is used only for authorized purposes, as specified by the patient’s consent and applicable regulations.
6. Data Modification: Any modifications to the data are logged and auditable.
7. Data Disposal: When data is no longer needed, it is securely disposed of according to regulations.

Tim Redaksi