Assessment Methods
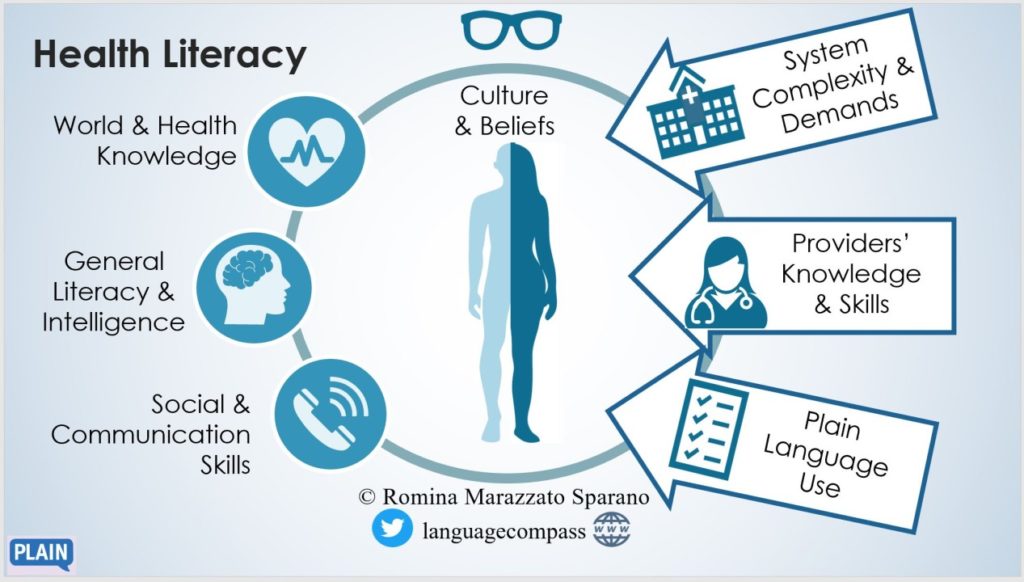
Assessing health literacy is crucial for effective healthcare communication and patient outcomes. A variety of methods exist, each with its own strengths and weaknesses, making the choice of assessment tool dependent on the specific context and target population. Understanding these methods and their limitations is vital for researchers and healthcare providers alike.
Several approaches are used to evaluate an individual’s health literacy. These include standardized tests, questionnaires, and observational methods. Each method offers a unique perspective on an individual’s ability to understand and utilize health information.
Standardized Tests
Standardized tests provide a structured and quantitative measure of health literacy. These tests typically involve reading comprehension tasks, numerical literacy questions, and questions assessing the ability to apply health information to real-world scenarios. Examples include the REALM (Rapid Estimate of Adult Literacy in Medicine) and the TOFHLA (Test of Functional Health Literacy in Adults). These tests offer a consistent and comparable measure across different populations, allowing for large-scale studies and comparisons. However, they can be time-consuming to administer and may not fully capture the nuances of health literacy, such as the ability to navigate the healthcare system or communicate effectively with healthcare providers. Furthermore, standardized tests may not be appropriate for all populations, particularly those with limited reading skills or cognitive impairments.
Questionnaires
Questionnaires offer a less intensive and often more flexible approach to assessing health literacy. These tools typically involve self-reported measures of health literacy skills and behaviors. They can be administered quickly and easily, making them suitable for large-scale surveys and screening purposes. Examples include the HLS-EU-Q (Health Literacy Scale for Europe Questionnaire) and the Newest Vital Sign (NVS). While questionnaires are cost-effective and easy to implement, they rely on self-reporting, which can be subject to bias and inaccuracies. Furthermore, questionnaires may not accurately reflect an individual’s actual health literacy skills, particularly if individuals overestimate or underestimate their abilities.
Observational Methods
Observational methods involve directly observing an individual’s interaction with health information and healthcare providers. This approach can provide valuable qualitative data on an individual’s health literacy skills in a real-world context. For example, researchers might observe a patient’s ability to understand medication instructions or follow a doctor’s advice. Observational methods offer a rich understanding of health literacy in action but are time-consuming, labor-intensive, and susceptible to observer bias. Furthermore, the setting of the observation might influence the results.
Key Elements of a Reliable and Valid Health Literacy Assessment Tool
A reliable and valid health literacy assessment tool should possess several key characteristics. Reliability refers to the consistency of the tool in measuring health literacy across different times and contexts. Validity refers to the extent to which the tool accurately measures what it intends to measure. Key elements include clear and concise instructions, items that are relevant to the target population, appropriate reading level, and a scoring system that is easy to interpret. The tool should also demonstrate good psychometric properties, including internal consistency and test-retest reliability. Furthermore, the tool should be culturally appropriate and accessible to diverse populations.
Comparison of Assessment Methods
| Assessment Method | Strengths | Weaknesses | Target Population |
|---|---|---|---|
| Standardized Tests (e.g., REALM, TOFHLA) | Standardized, comparable results; quantitative data | Time-consuming; may not capture all aspects of health literacy; may be inaccessible to some populations | Adults with varying literacy levels |
| Questionnaires (e.g., HLS-EU-Q, NVS) | Quick, easy to administer; cost-effective; can screen large populations | Relies on self-report; may not accurately reflect actual skills | Adults with varying literacy levels; adaptable to specific populations |
| Observational Methods | Provides rich qualitative data; observes real-world application of health literacy | Time-consuming; labor-intensive; susceptible to observer bias | Individuals in specific healthcare settings; can be tailored to various populations |
Interpreting Assessment Results: How Tdo You Assess Health Literacy
Interpreting the results of a health literacy assessment involves more than just looking at a raw score. It requires a nuanced understanding of the individual’s performance in relation to their specific context, including their health status, cultural background, and educational experiences. Accurate interpretation allows for the development of effective, targeted interventions that truly address the individual’s needs.
Understanding the assessment’s scoring system is crucial. Many assessments provide a range of scores, often categorized into levels representing different levels of health literacy. For example, a score might indicate “adequate,” “marginal,” or “low” health literacy. However, it’s important to remember that these are broad classifications, and the specific challenges faced by individuals within each category can vary greatly. The assessment should also ideally provide detailed information on areas of strength and weakness.
Using Assessment Data to Develop Targeted Interventions
Assessment data provides a roadmap for creating personalized interventions. A low score on medication comprehension, for example, suggests the need for interventions focused on improving understanding of medication instructions. This could involve using simpler language, visual aids, or interactive tools. Conversely, a strength in accessing health information online might suggest incorporating digital health tools into the intervention plan. The goal is to build upon existing strengths while addressing specific weaknesses identified by the assessment. The intervention should be tailored to the individual’s learning style and preferences, taking into account factors such as their age, language proficiency, and cultural background.
The Importance of Context in Interpreting Assessment Results
The context surrounding the assessment is paramount. A low health literacy score obtained by an elderly individual with limited formal education and recent vision impairment might have different implications than a similar score from a young adult with a college degree. Factors such as language barriers, cognitive impairments, and psychosocial stressors can all significantly impact an individual’s performance on a health literacy assessment. Therefore, it’s crucial to consider these factors when interpreting the results and designing interventions. A holistic approach that addresses the individual’s overall circumstances is essential for effective intervention.
Hypothetical Case Study: Developing an Intervention Plan
Consider Mrs. Jones, a 72-year-old woman with type 2 diabetes who scored in the “low” range on a health literacy assessment. The assessment revealed significant difficulty understanding her medication regimen and blood glucose monitoring instructions. Furthermore, she reported limited computer skills and relied heavily on family members for support. Her context included low vision and a recent bereavement that affected her motivation.
Based on these results, a tailored intervention could involve:
- Simplified medication instructions with large print and visual aids (e.g., a pill organizer with clear labeling).
- Hands-on training with a diabetes educator on blood glucose monitoring using a simplified device with large display and audible prompts.
- In-person education sessions using simple language and visual aids, conducted in a comfortable and familiar setting.
- Referral to support groups for peer interaction and emotional support to address the impact of bereavement on her health management.
This intervention directly addresses Mrs. Jones’ specific challenges, acknowledging her limited literacy skills, vision impairment, and recent emotional distress. The intervention is also designed to be accessible and supportive, enhancing her ability to manage her diabetes effectively.
Impact of Health Literacy on Healthcare Systems
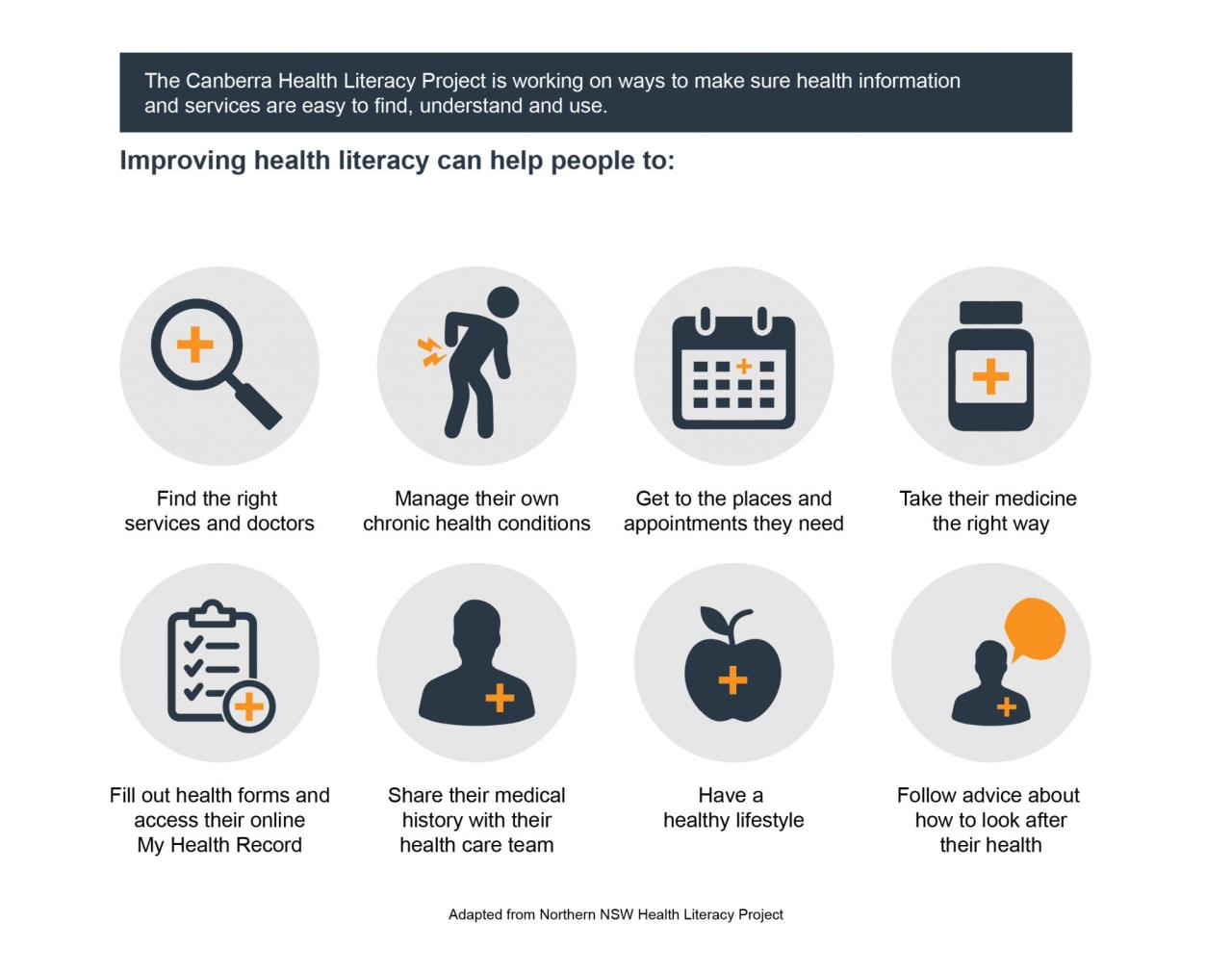
Health literacy, or the ability to understand and use health information, significantly impacts the efficiency and effectiveness of healthcare systems. Low health literacy contributes to increased healthcare costs and suboptimal utilization of services, while improvements in health literacy lead to better patient outcomes and a more sustainable healthcare environment. This section explores the multifaceted relationship between health literacy and the overall functioning of healthcare systems.
Low health literacy correlates with higher healthcare costs and increased utilization of services. Individuals with limited health literacy often struggle to manage their chronic conditions effectively, leading to more frequent hospitalizations, emergency room visits, and greater reliance on expensive specialized care. They may also be less likely to adhere to prescribed medication regimens or follow preventative health recommendations, resulting in more costly treatments for preventable complications. For example, studies have shown a strong link between low health literacy and higher rates of hospital readmissions for conditions like heart failure and diabetes. This increased utilization of healthcare resources directly translates to higher overall healthcare expenditures.
The Correlation Between Low Health Literacy and Increased Healthcare Costs
Studies consistently demonstrate a positive correlation between low health literacy and increased healthcare costs. Patients with poor health literacy are more likely to experience preventable hospitalizations and emergency room visits, contributing significantly to escalating healthcare expenses. Their difficulties in understanding medical instructions and managing their conditions lead to complications that require more extensive and costly interventions. For instance, a patient with low health literacy might miss crucial details about medication dosages or follow-up appointments, resulting in adverse health events and increased healthcare utilization. This ultimately places a substantial burden on the healthcare system and its financial resources.
Improved Health Literacy and Enhanced Health Outcomes
Conversely, improved health literacy empowers individuals to make informed decisions about their health, leading to better health outcomes and reduced healthcare costs. When patients understand their conditions, treatment plans, and self-management strategies, they are more likely to adhere to their prescribed regimens, participate actively in their care, and make healthier lifestyle choices. This proactive approach to health management reduces the likelihood of preventable complications and hospitalizations, thus lowering healthcare utilization and expenses. For example, interventions aimed at improving diabetes self-management education among low-literacy populations have demonstrated significant improvements in blood glucose control and reduced hospital readmissions.
Examples of Successful Health Literacy Interventions at the System Level
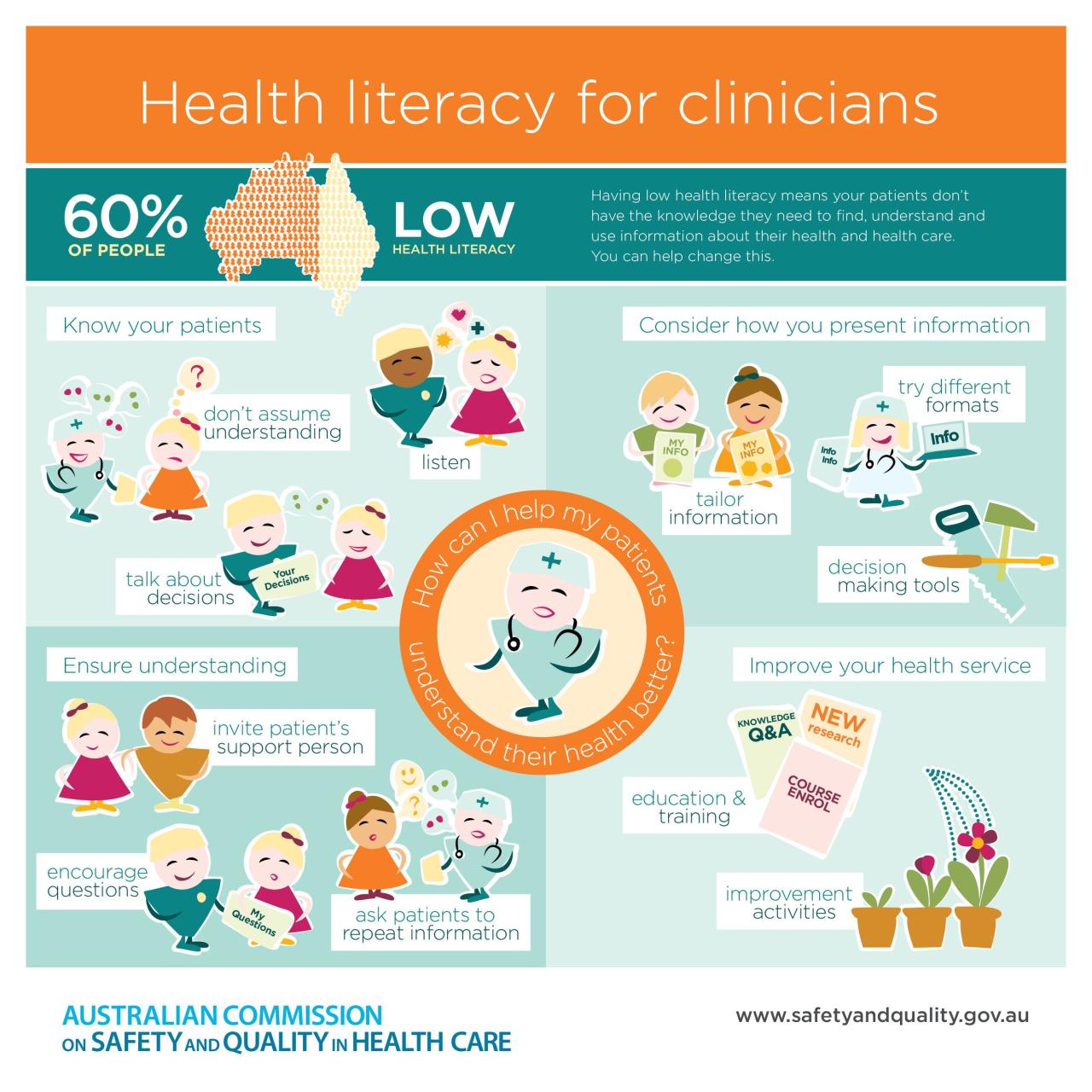
Several successful health literacy interventions have been implemented at the system level, demonstrating the potential for positive change. These interventions often involve multifaceted approaches that address various aspects of healthcare delivery. For example, some healthcare systems have implemented plain language materials and patient education programs tailored to different literacy levels. Others have incorporated visual aids, interactive tools, and technology-based solutions to improve patient understanding. The use of teach-back methods, where healthcare providers verify patient comprehension by asking them to explain the information in their own words, is another effective strategy. These system-wide changes contribute to a more equitable and effective healthcare system for all.
The Role of Health Policy in Promoting Health Literacy, How tdo you assess health literacy
Health policy plays a crucial role in promoting health literacy across the population. Policies can incentivize healthcare providers to incorporate health literacy best practices into their daily work. For example, reimbursement models could reward providers for delivering patient-centered care that prioritizes clear communication and shared decision-making. Furthermore, policies can support the development and dissemination of health information resources that are accessible and understandable for all individuals, regardless of their literacy levels. Investing in health literacy initiatives through policy changes can lead to significant improvements in population health and reduced healthcare costs in the long term. For instance, mandatory training programs for healthcare professionals on effective communication strategies could contribute to a culture of health literacy within the healthcare system.

Tim Redaksi